Enhancing Mental Health Through Fermented Foods and Gut Microbiome
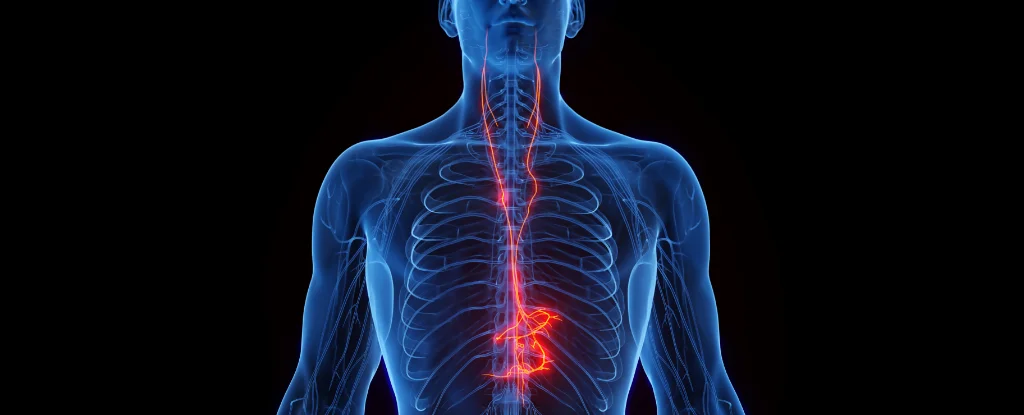
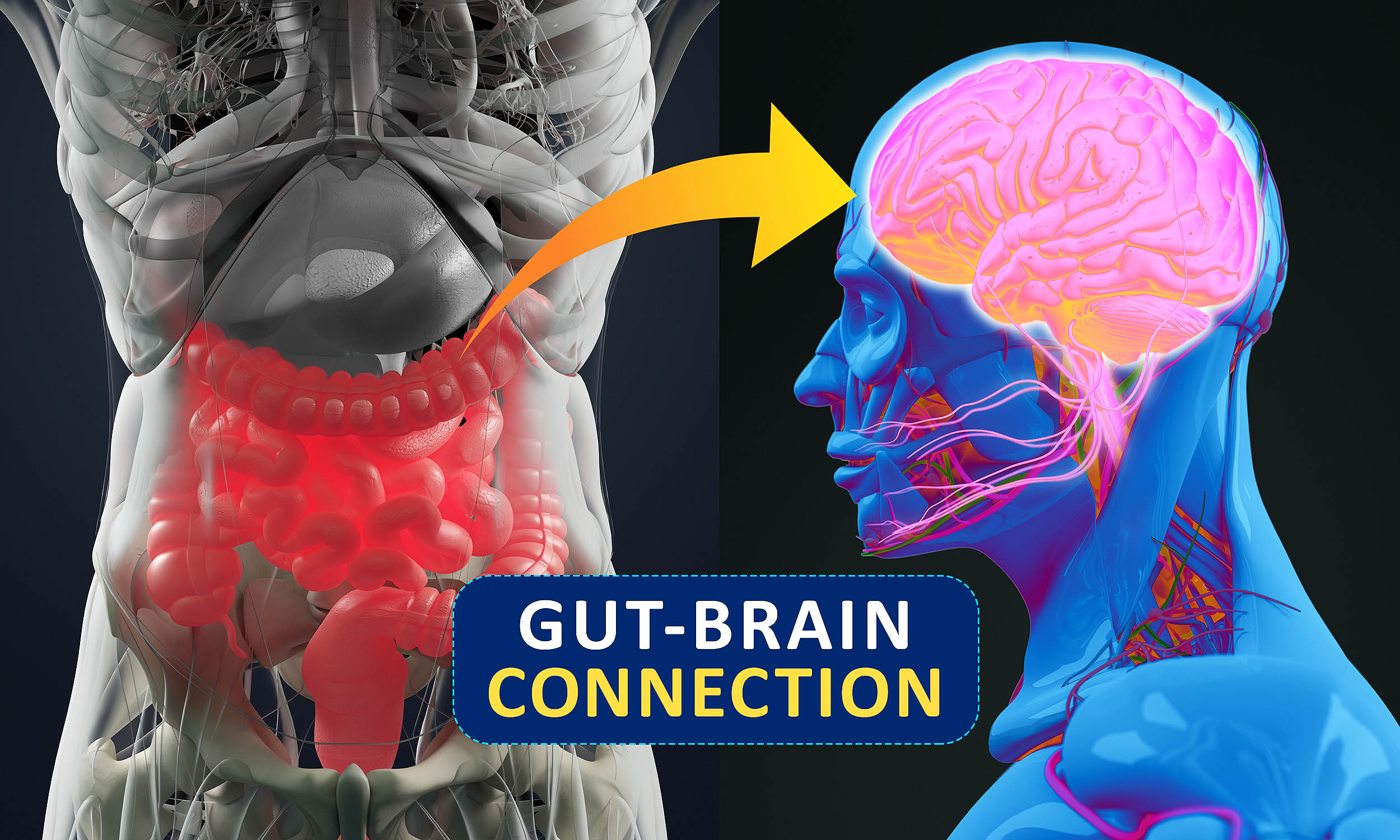
Eating fermented foods like yogurt, kefir, and sauerkraut can support gut health by providing probiotics, which in turn can enhance the gut-brain connection, potentially improving mood, stress regulation, and sleep. Incorporating these foods into your diet is simple and beneficial for overall health.