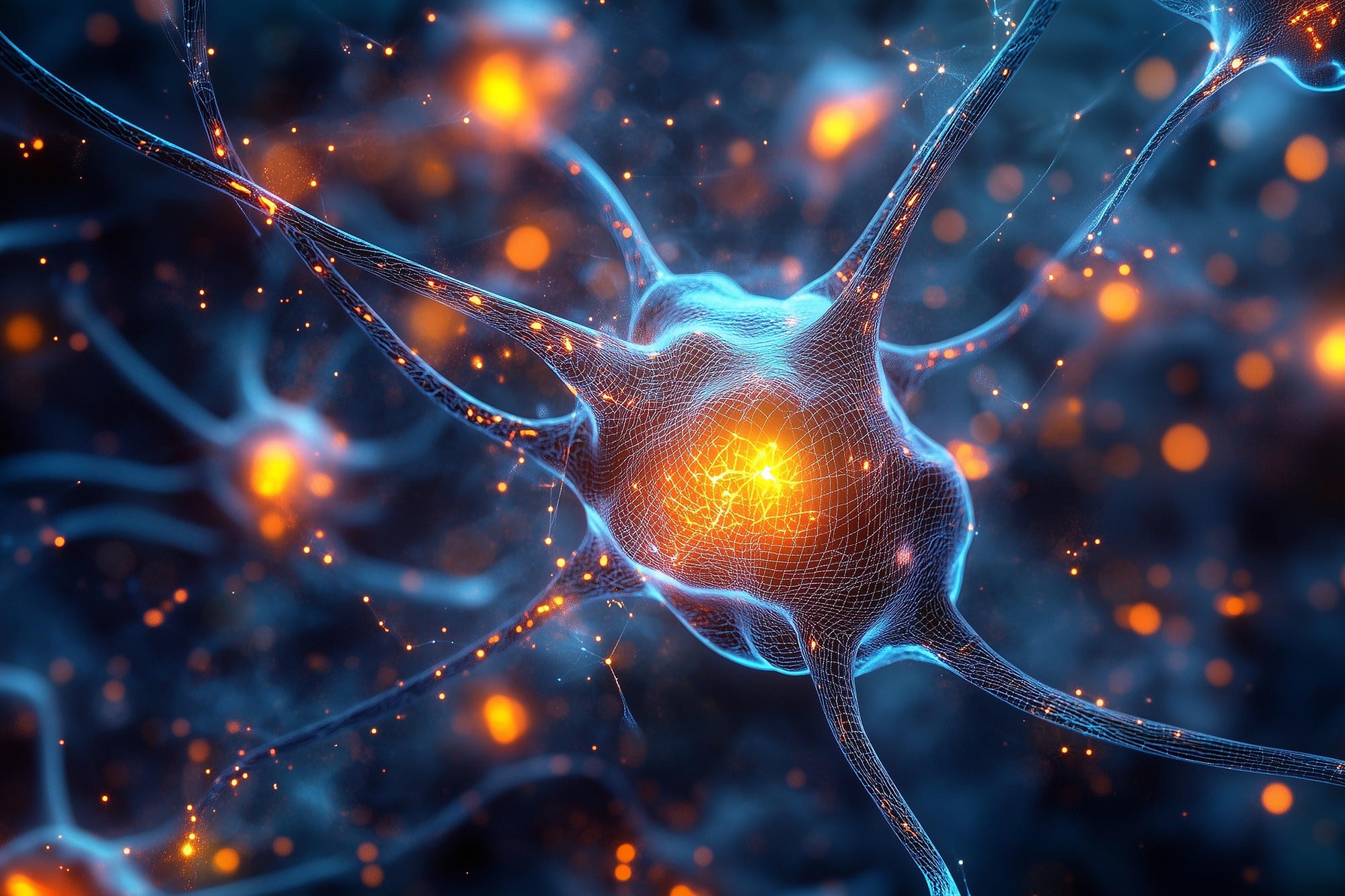
Aging brain's slow protein recycling may fuel synapse decline tied to Alzheimer's
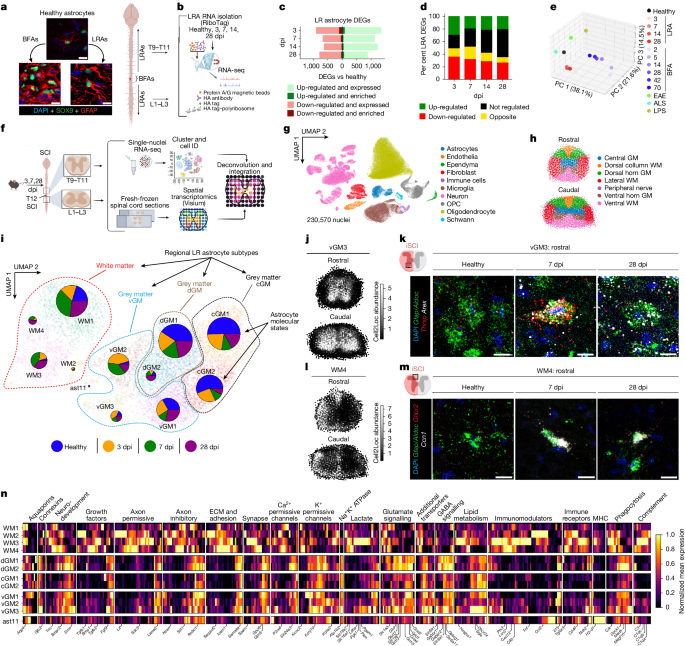
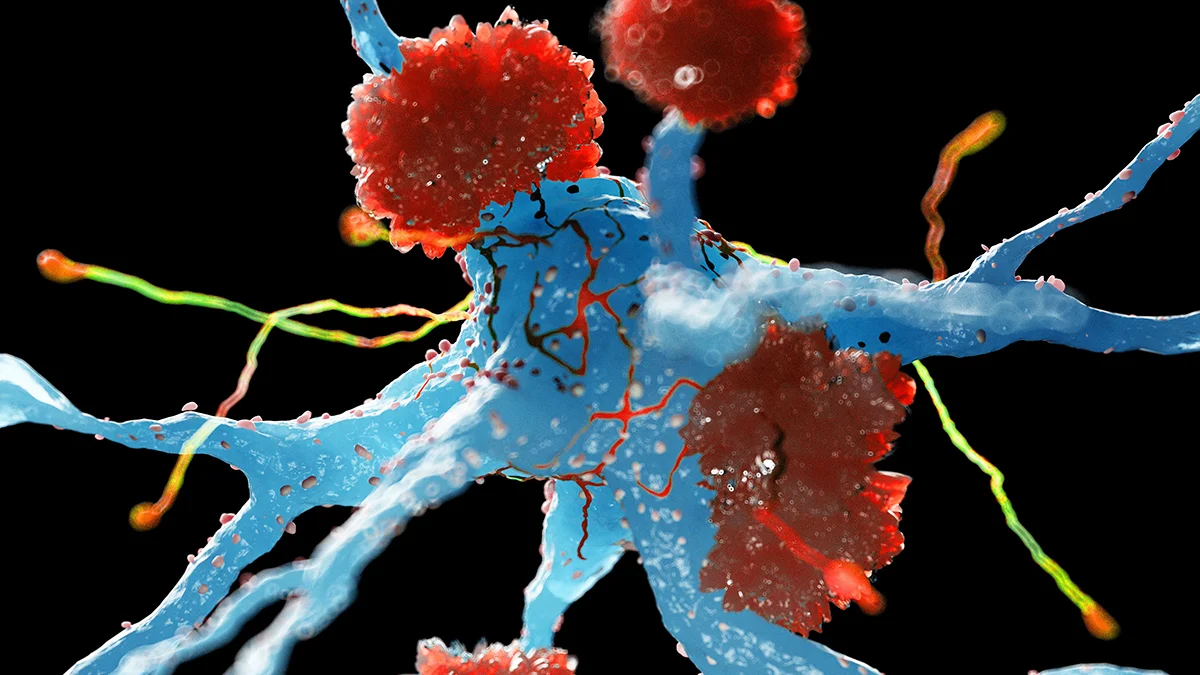
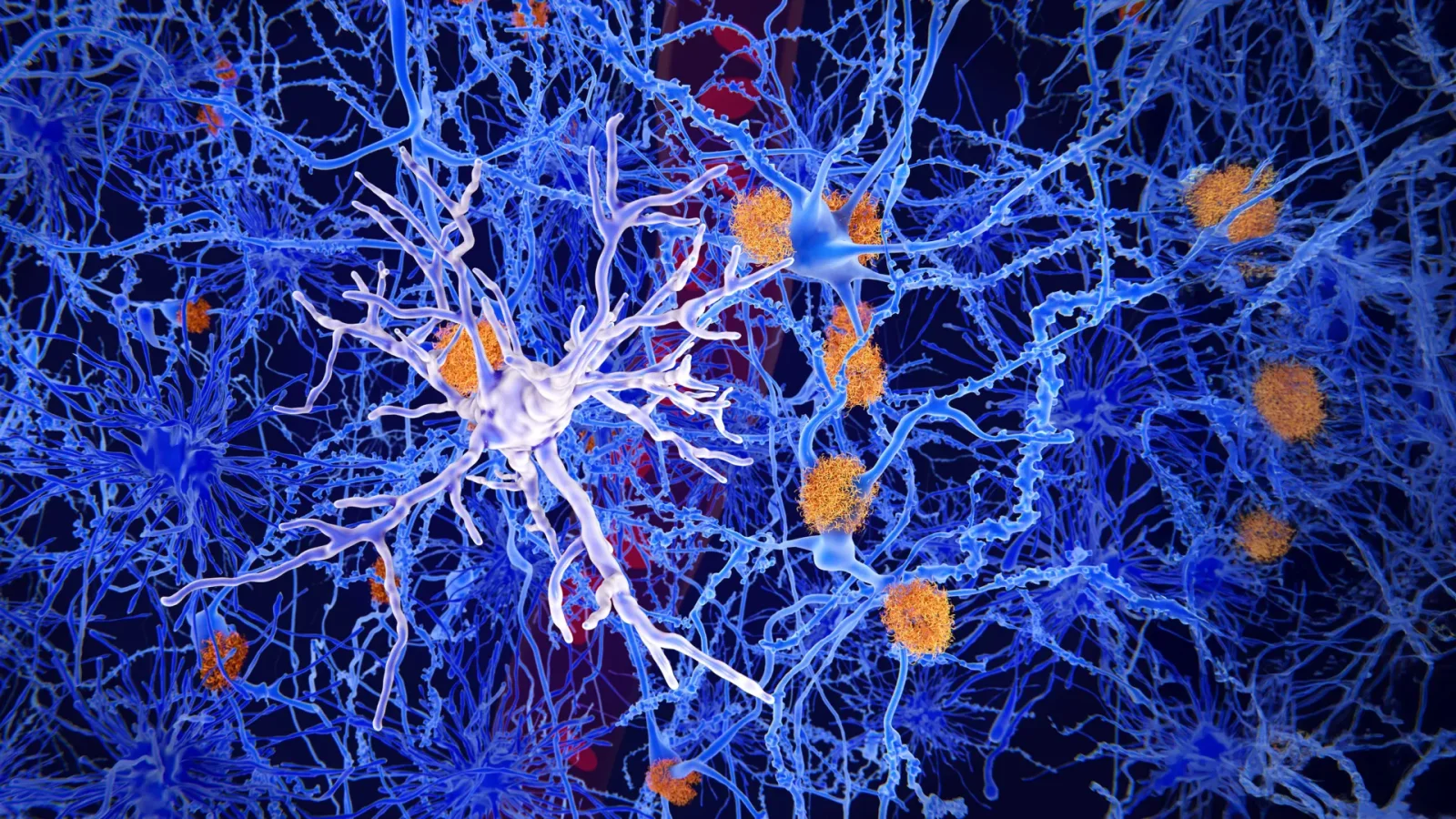
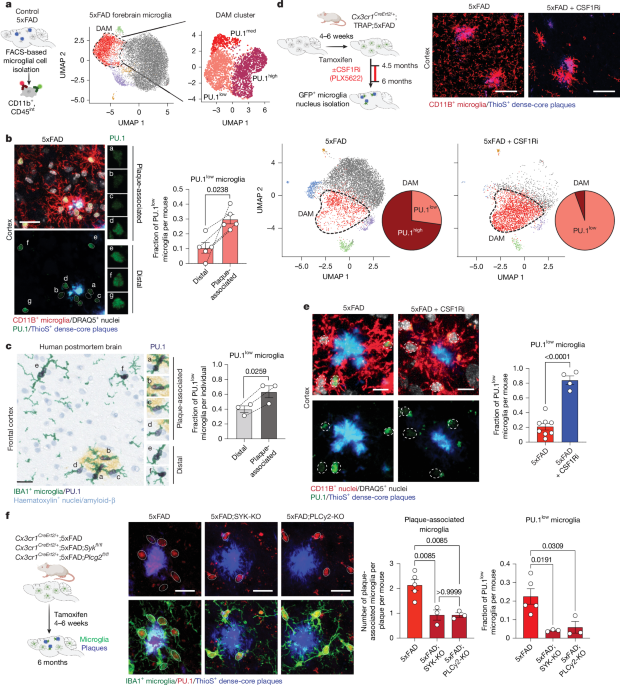
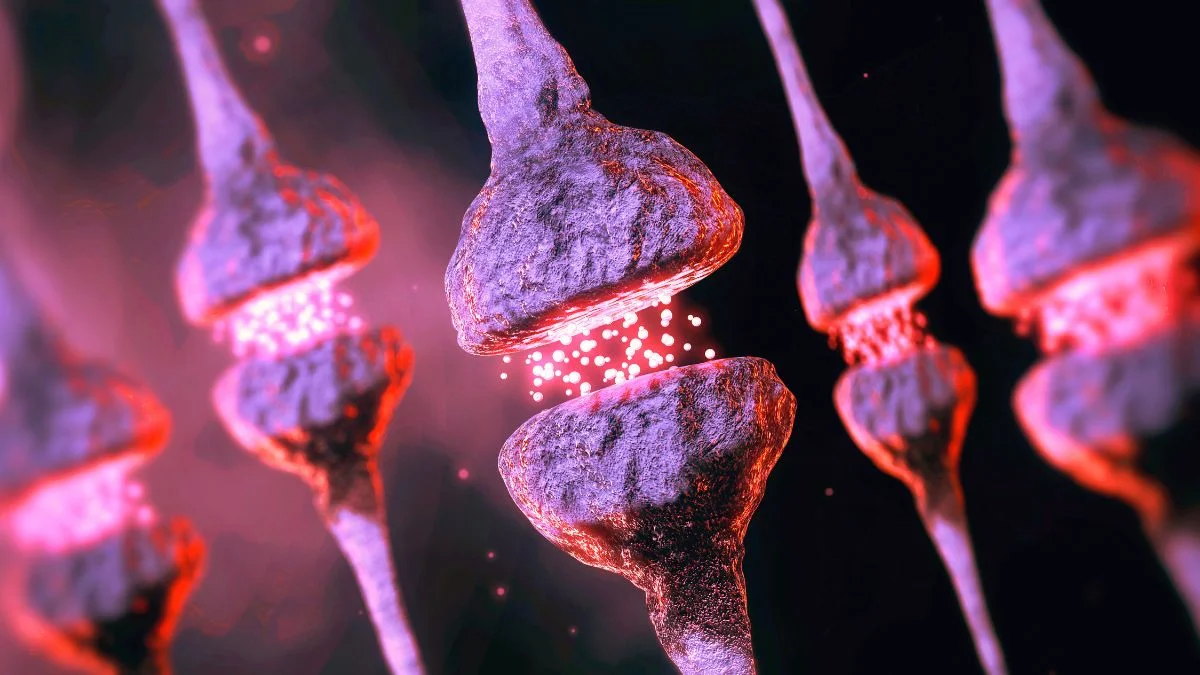
Age-related slowdown of neuronal protein recycling leads to protein clumps at synapses; microglia attempt cleanup but can become overwhelmed, potentially impairing neuron communication and linking aging to synaptic loss and higher neurodegenerative risk, with new targets for therapy and biomarkers suggested.