Pill-Based Donor Microbes Show Early Promise in Boosting Cancer Immunotherapy
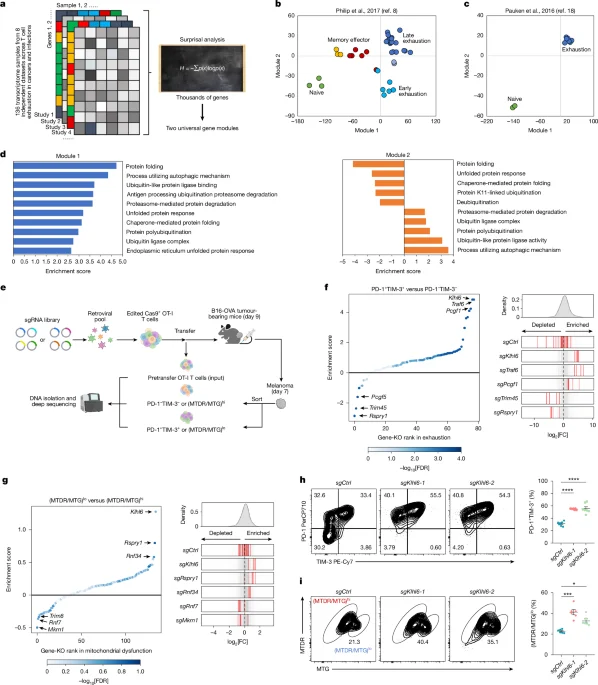
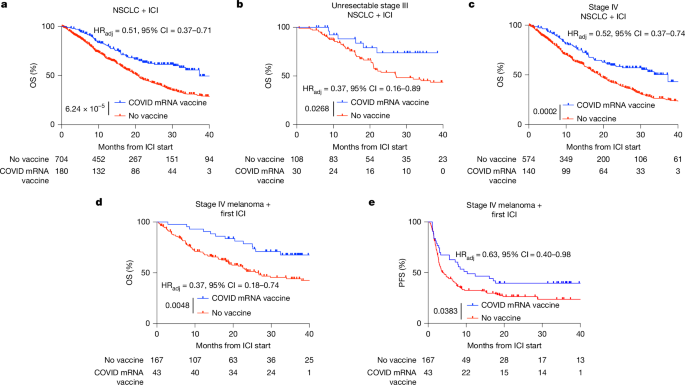
Two small Nature Medicine trials suggest oral fecal microbiota transplantation (FMT) pills may boost immunotherapy in advanced cancers: in metastatic kidney cancer, FMT reduced immunotherapy side effects and produced about a 50% response; in advanced lung cancer or melanoma, combining FMT with immunotherapy yielded response rates around 75–80%, higher than typical 39–45% rates. While promising, results are early and require larger trials.