Five-day brain-stimulation therapy sparks remission in some with treatment-resistant depression
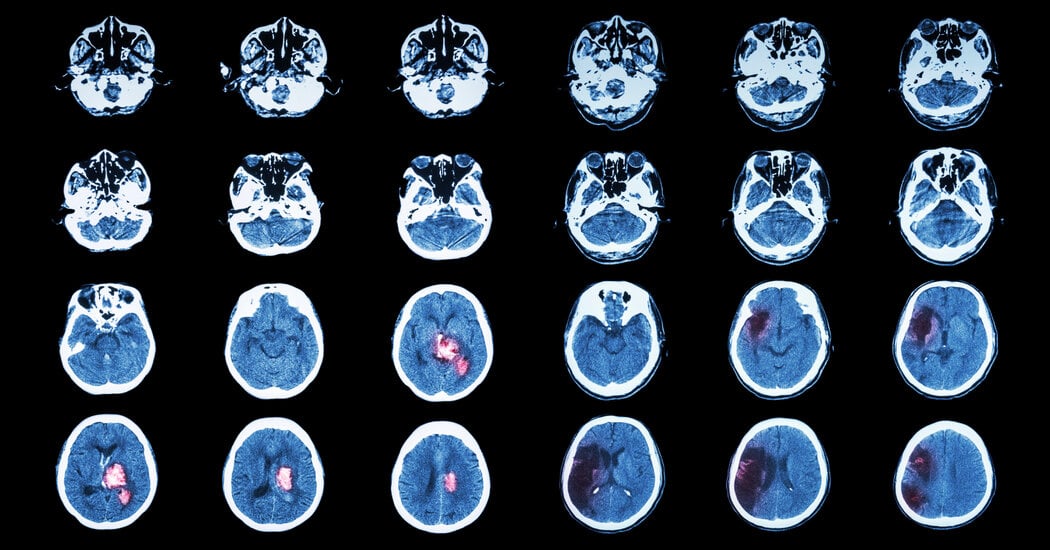
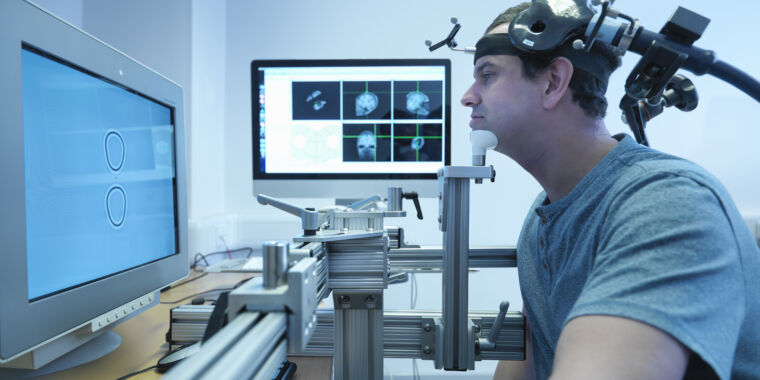
A Stanford-led study tests SAINT (Stanford Accelerated Intelligent Neuromodulation Therapy), a five-day, high-precision, noninvasive brain-stimulation treatment for treatment-resistant depression. In the trial, about half of the 24 participants receiving SAINT remitted by one month, compared with about 21% in the placebo group. SAINT uses rapid magnetic pulses targeted at the left dorsolateral prefrontal cortex via ten 10-minute sessions per day, delivering treatment faster and with greater precision than conventional TMS; the FDA cleared SAINT in 2022 and it’s offered at about 17 US clinics, though costs range roughly $16,000-$30,000 and insurance coverage varies. EEG data hint at biomarkers that could help predict who benefits, but more diverse studies are needed to confirm durability and broader applicability.