California Faces a Vaccine-Free HMPV Surge: Key Facts for the Public
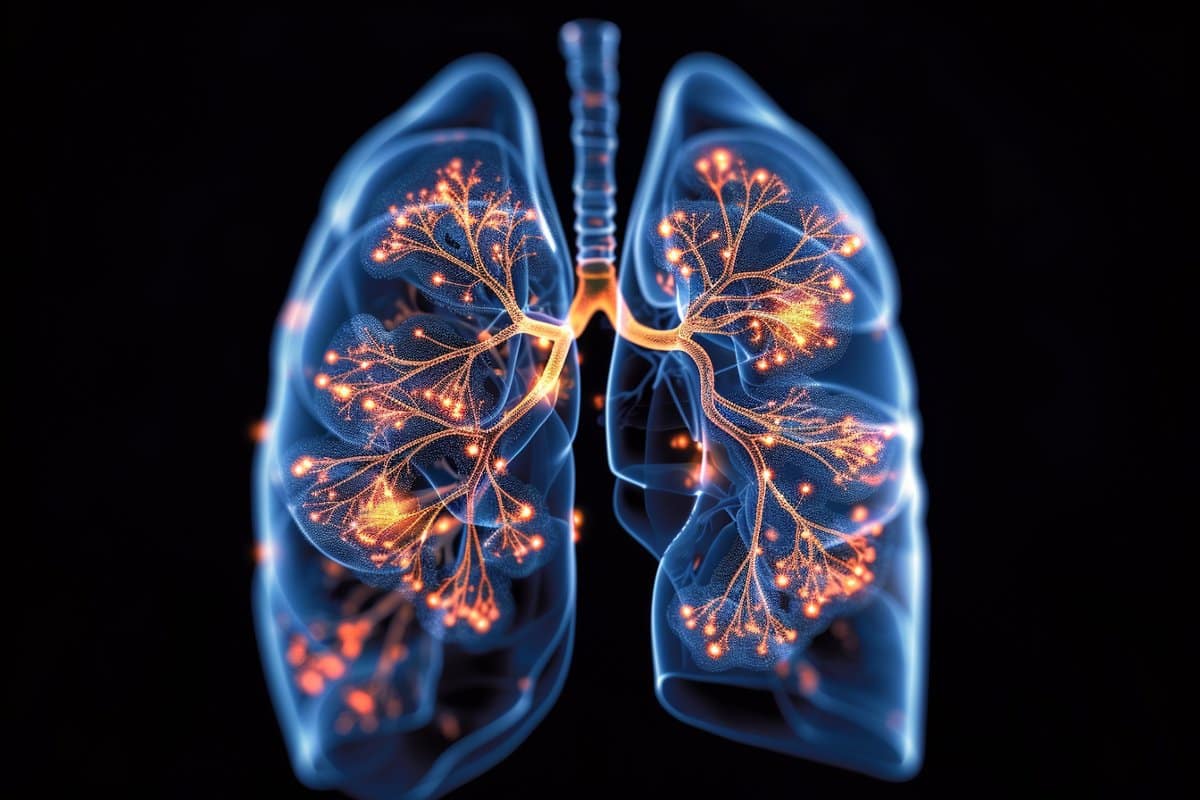
Public health experts warn that a vaccine-free human metapneumovirus (HMPV) is rising in Northern California, with wastewater data showing high levels in cities like Redwood City and broader spread along the Bay Area and Napa. National cases have been trending up since October 2025. HMPV typically causes cold-like symptoms but can lead to more serious issues such as wheezing, asthma attacks, middle-ear infections, pneumonia, and, in vulnerable individuals, death. There is no vaccine to prevent HMPV; prevention focuses on handwashing, cleaning surfaces, staying home when sick, and seeking medical care if symptoms worsen. Most people recover with rest and fluids, with treatment in severe cases including oxygen, steroids, and IV fluids as needed.