Selective 'mirror' amino acid inhibits specific tumor growth
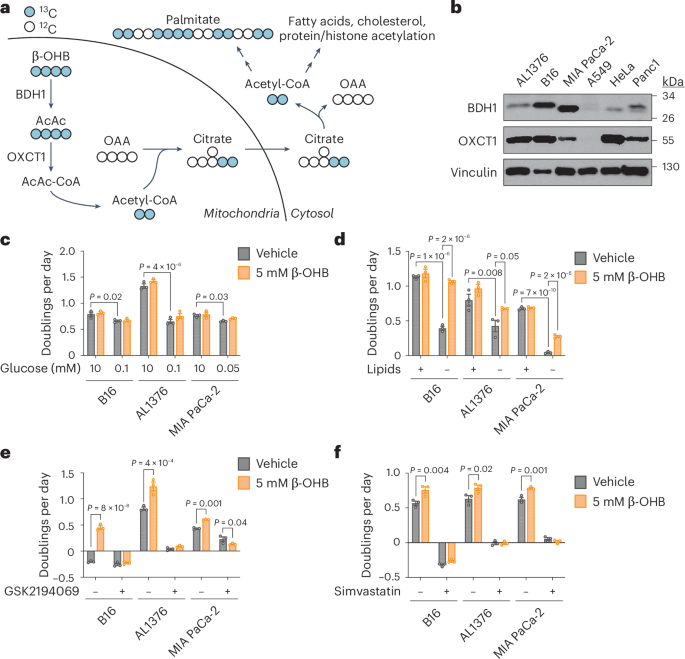
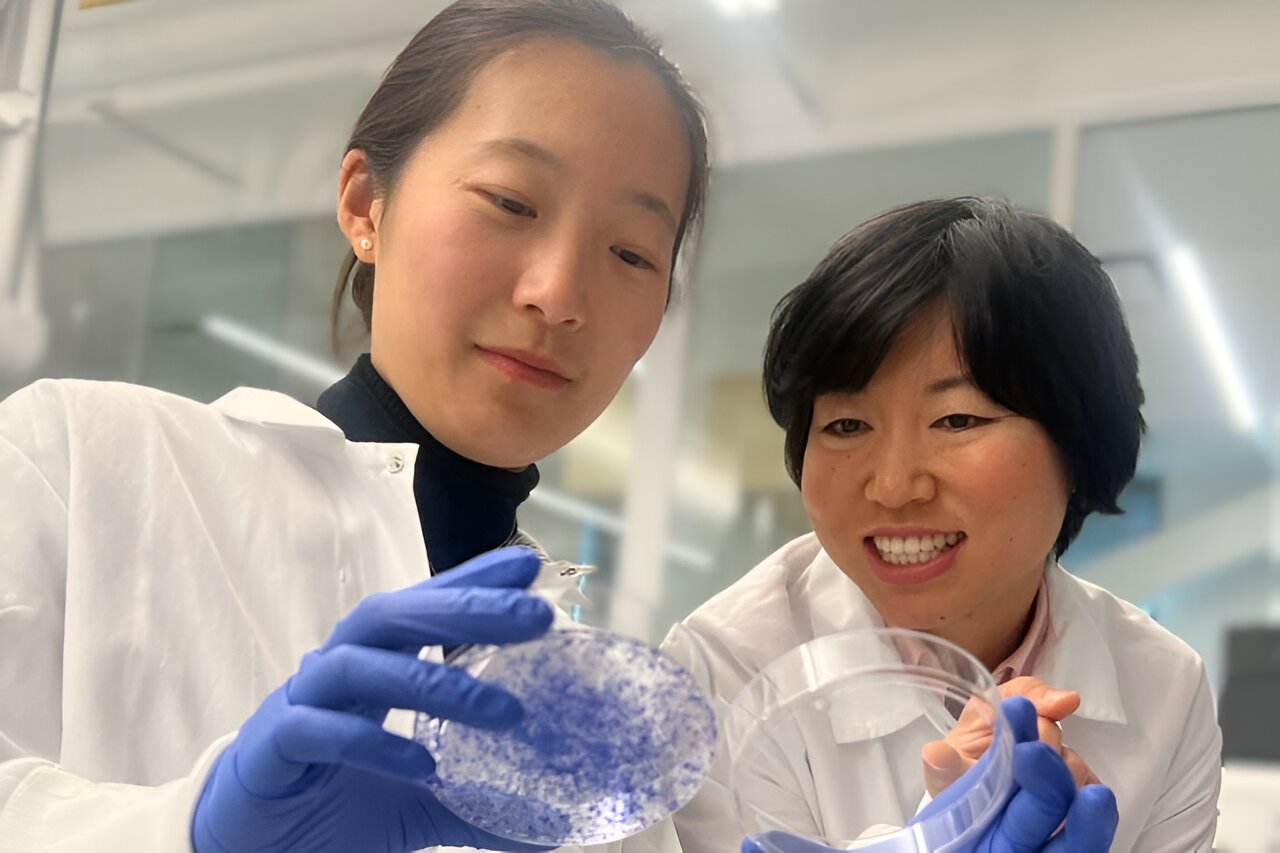
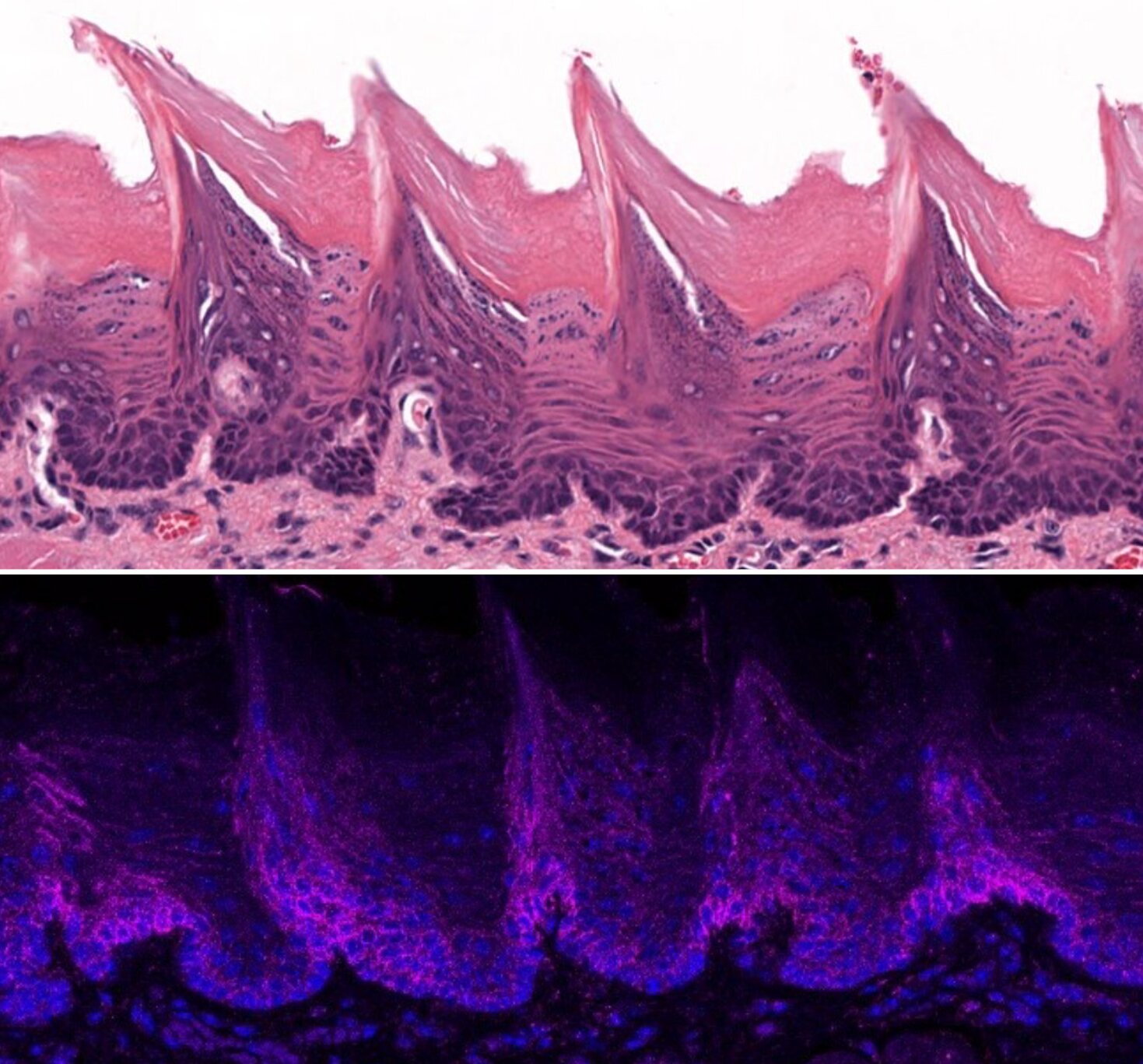
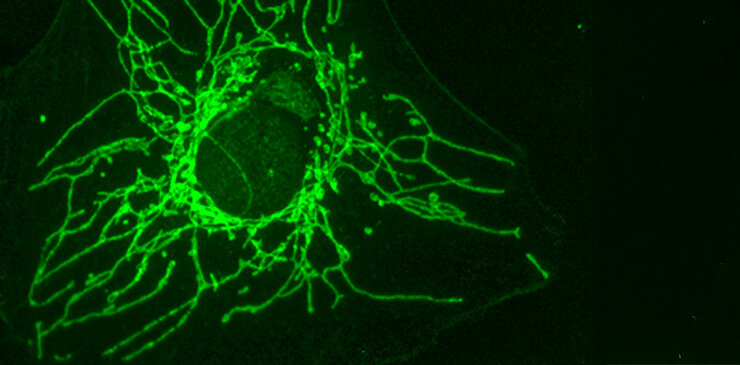
Researchers have discovered that D-cysteine, a mirror form of the amino acid cysteine, selectively inhibits the growth of certain cancer cells by blocking a key mitochondrial enzyme, showing promise for targeted cancer therapies with minimal effects on healthy cells, as demonstrated in mouse models.