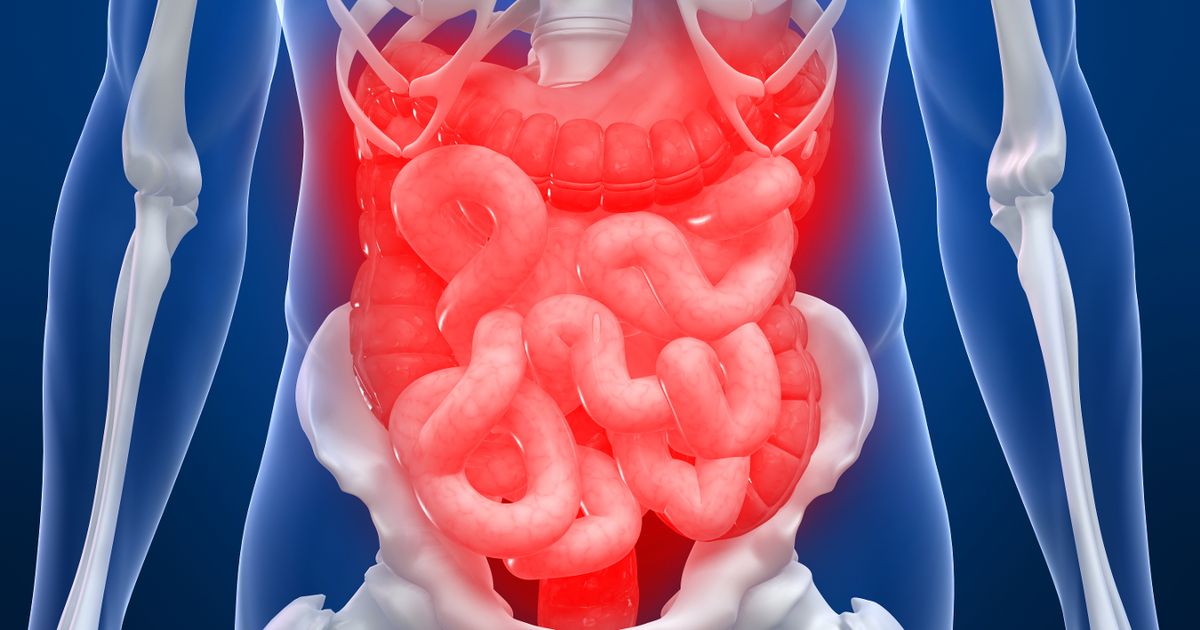
ER dismissal, then rectal cancer: a Toronto model’s urgent cancer journey
Toronto model Jess Grossman, who lives with an ostomy after childhood Crohn’s disease and colon removal, says ER staff brushed off her persistent pelvic pain as endometriosis until a CT scan raised flags. After a biopsy, she was diagnosed with rectal cancer four weeks from the first symptoms and is undergoing eight rounds of chemotherapy (16 weeks total) to shrink the tumor before potential surgery to remove the rectal stump. She documents her journey online to raise awareness about colorectal cancer and the importance of early detection.