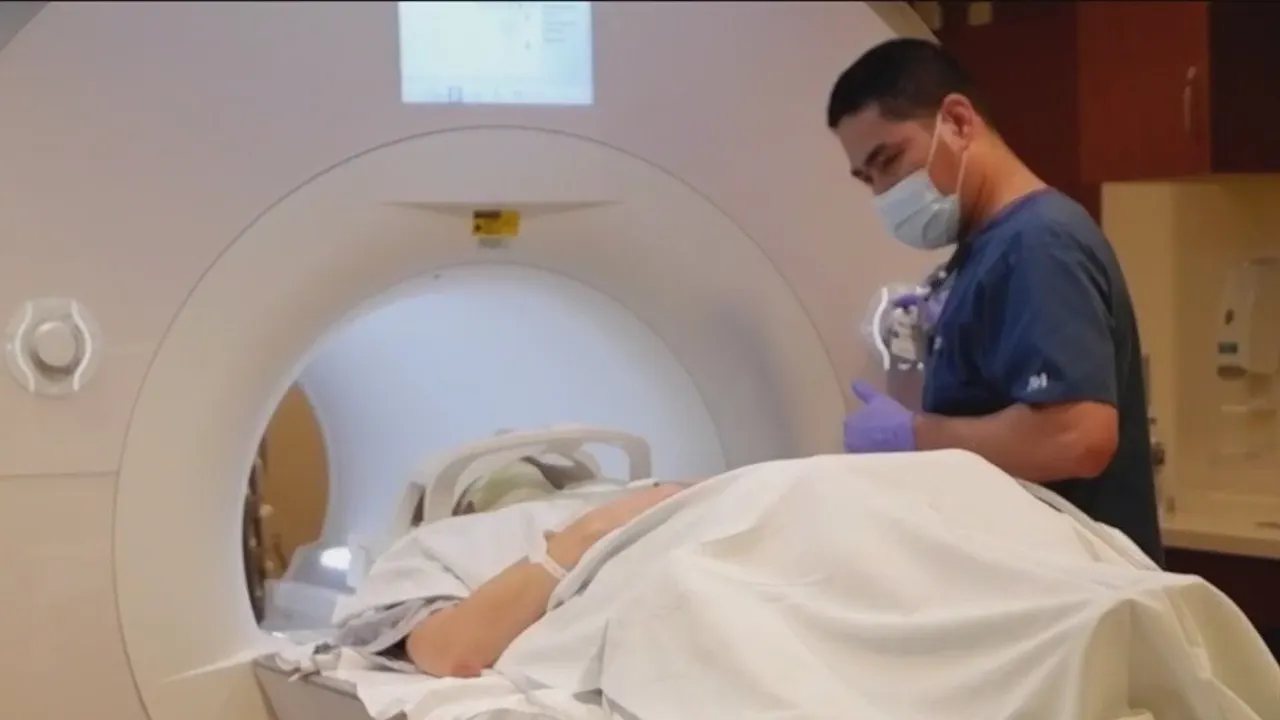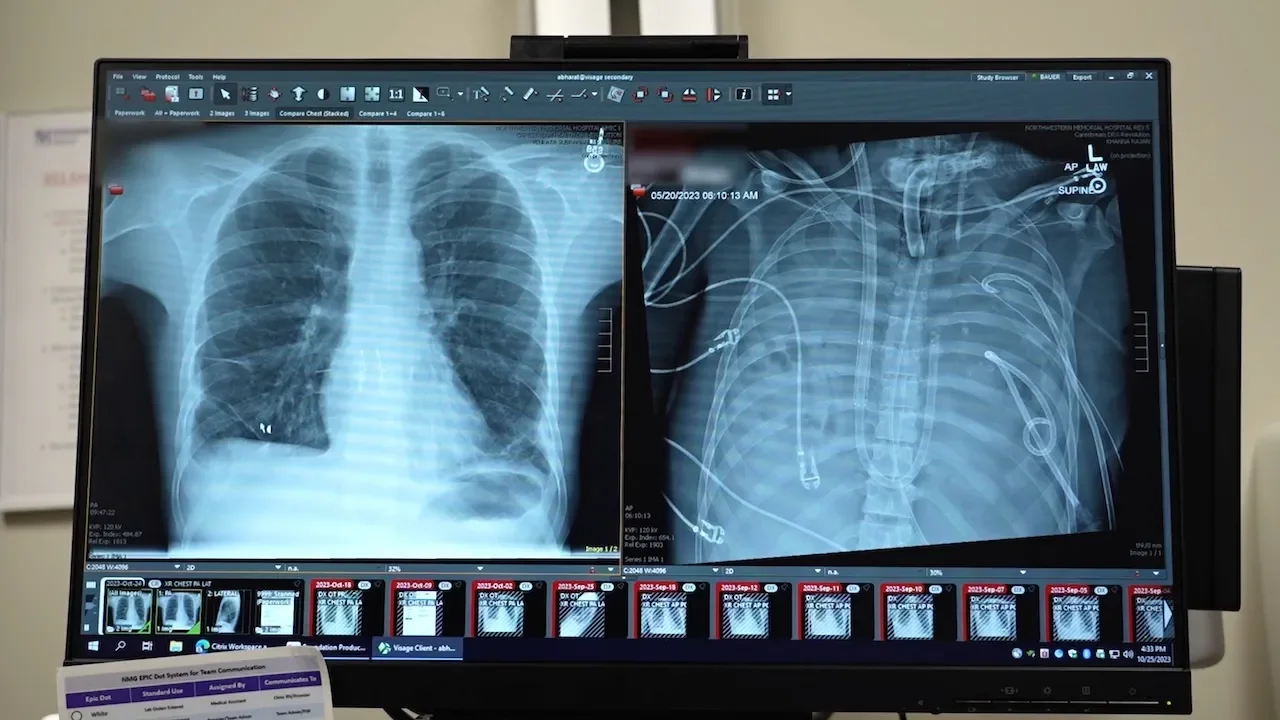
Patient survives 48 hours on a total artificial lung before double-lung transplant
Surgeons at Northwestern Medicine used a total artificial lung system to take over gas exchange after removing both diseased lungs from a critically ill patient, preserving heart function and bridging him to a double-lung transplant. The patient survived 48 hours on life support and, after the procedure, recovered well; two years later he has normal lung function and is fully independent.