"12,000-Year-Old Preserved Human Brains Challenge Soft Tissue Decay Assumptions"
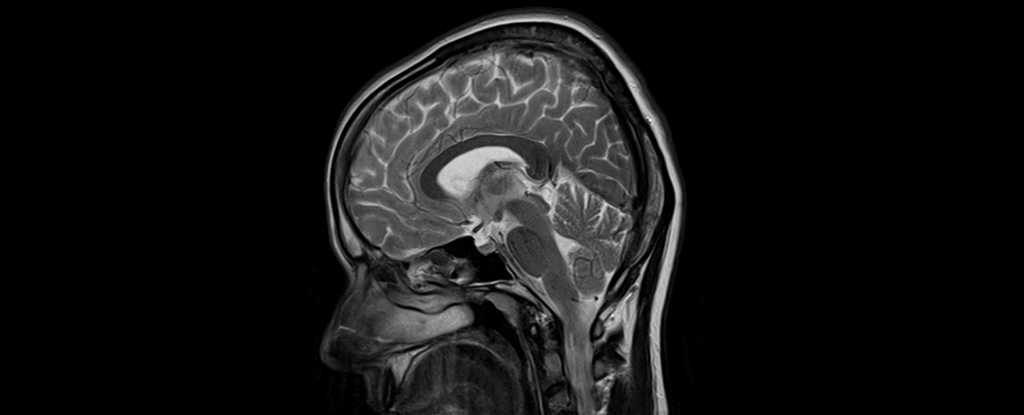
A global archive of over 4,400 preserved human brains, some dating back 12,000 years, has provided groundbreaking insight into soft tissue preservation, challenging the perception that naturally preserved brains are extremely rare. The brains, originating from various environments worldwide, were found to have been preserved through mechanisms such as dehydration, freezing, saponification, and tanning. This research could offer valuable information on human evolution, ancient health, and diseases, including neurodegenerative conditions like Alzheimer's. The study highlights the need for excavating archaeologists to remain open to unexpected discoveries and emphasizes the scientific value of studying these preserved human remains.