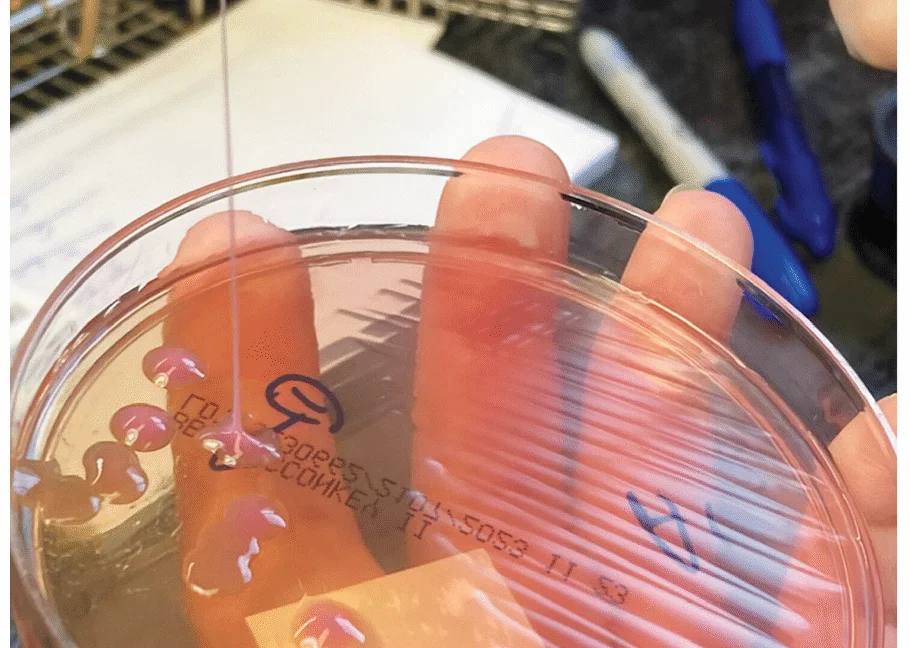
Hypervirulent Klebsiella pneumoniae floods the body, destroying an eye
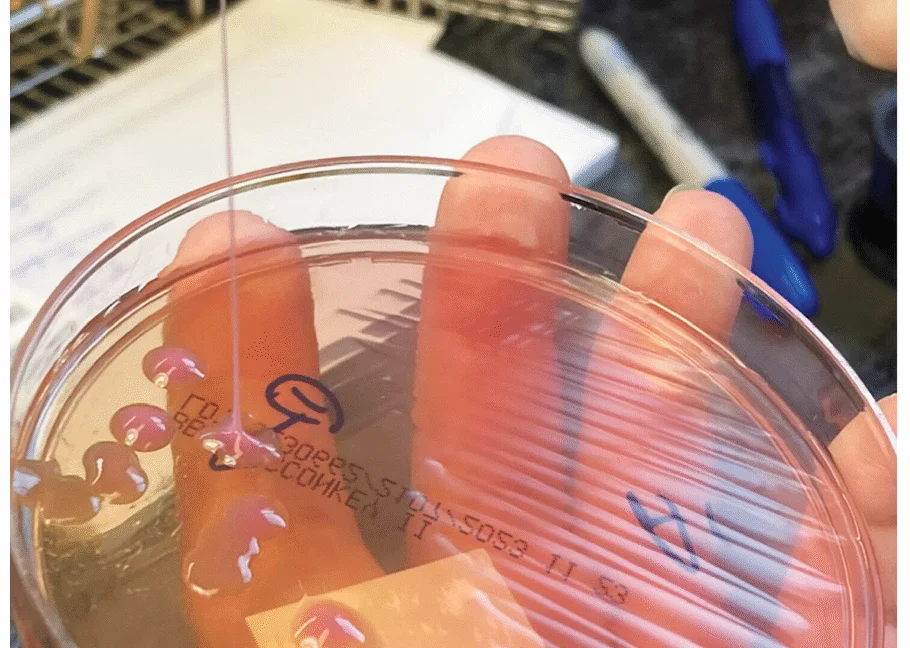
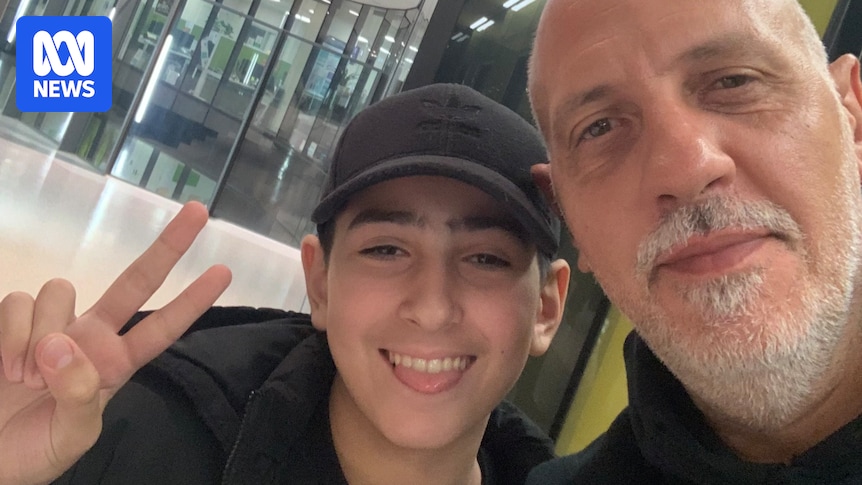
A generally healthy 63-year-old man in New England developed a metastatic infection from hypervirulent Klebsiella pneumoniae, with liver abscesses, lung nodules, brain lesions, and a rapidly progressive endogenous endophthalmitis that led to the removal of his right eye. Diagnosis relied on virulence markers and a simple string test, and despite a nine-month course of antibiotics, the eye could not be saved. The liver abscesses resolved and brain lesions largely shrank, underscoring hvKP as a rising global threat, though this patient’s strain was not highly antibiotic-resistant.