Nasal Nanodrops Show Promise in Treating Brain Tumors
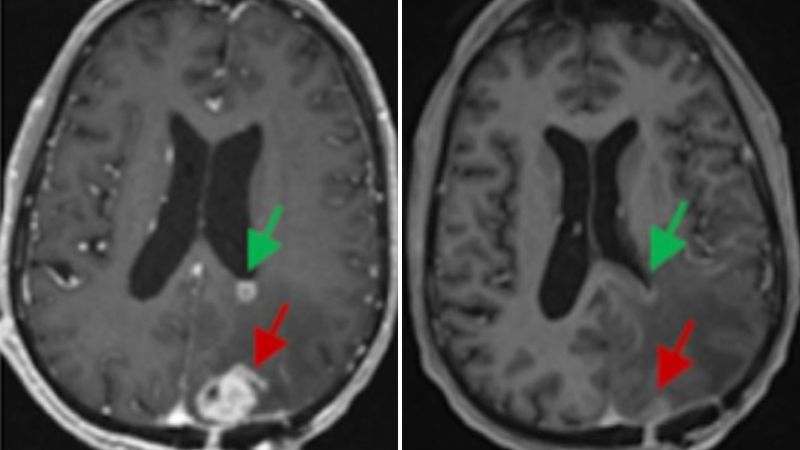
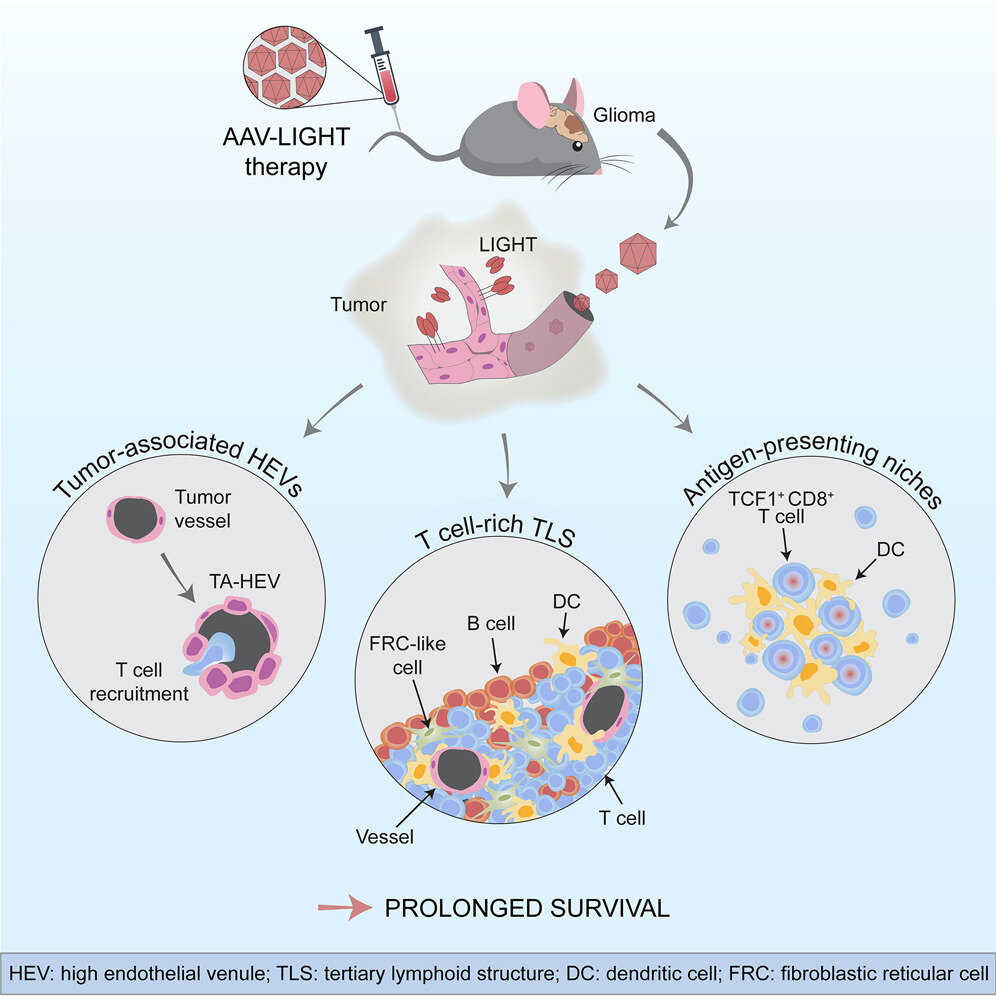
Researchers have developed a noninvasive nasal nanotherapy using gold-based spherical nucleic acids that successfully eradicated glioblastoma tumors in mice by activating immune pathways, offering a promising new approach for treating deadly brain cancers.