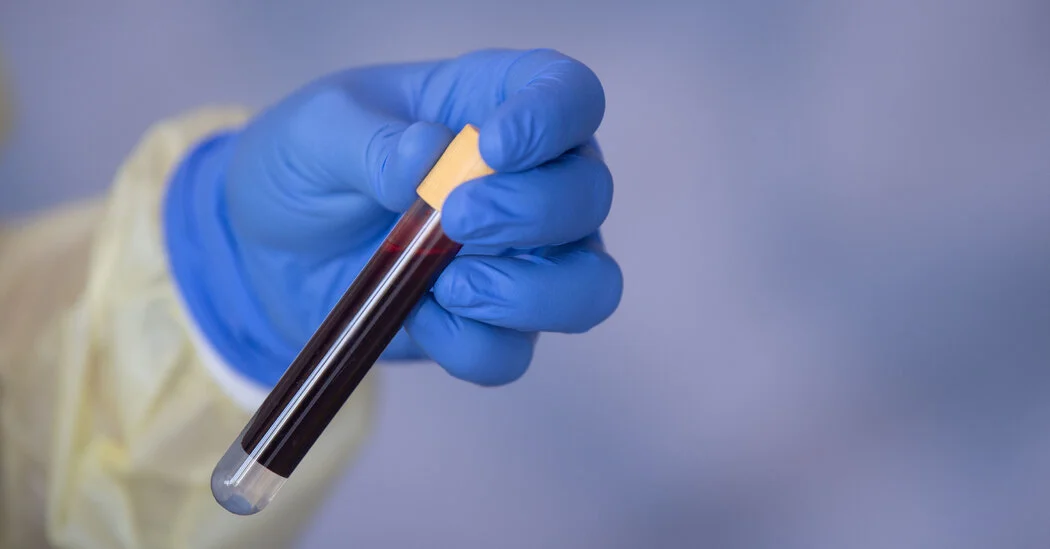
Major UK Trial Undermines Promise of Galleri Multi-Cancer Blood Test
In a large UK trial of 142,000 adults over three years, Grail's Galleri multi-cancer blood test did not reduce late-stage cancers (stages 3–4), though researchers noted a secondary signal of fewer Stage 4 cancers; the test remains FDA-unapproved, is sold with limited insurer coverage, and Medicare coverage remains under legislative review.