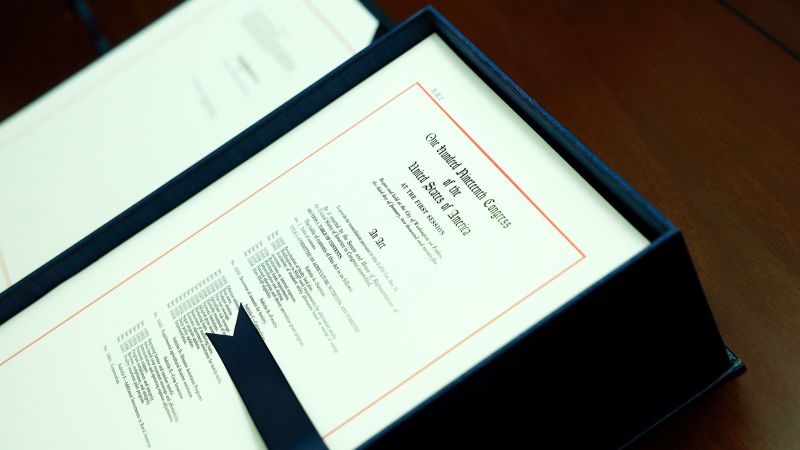
Trump administration launches $50B rural health funding with conditions
The Trump administration announced a $10 billion rural health fund for 2026, with funds distributed based on population, health outcomes, and policy compliance, including restrictions on SNAP benefits. Critics argue the funding is insufficient to offset the massive Medicaid cuts and that the allocation may be influenced by political policies, potentially limiting aid to rural hospitals in need.