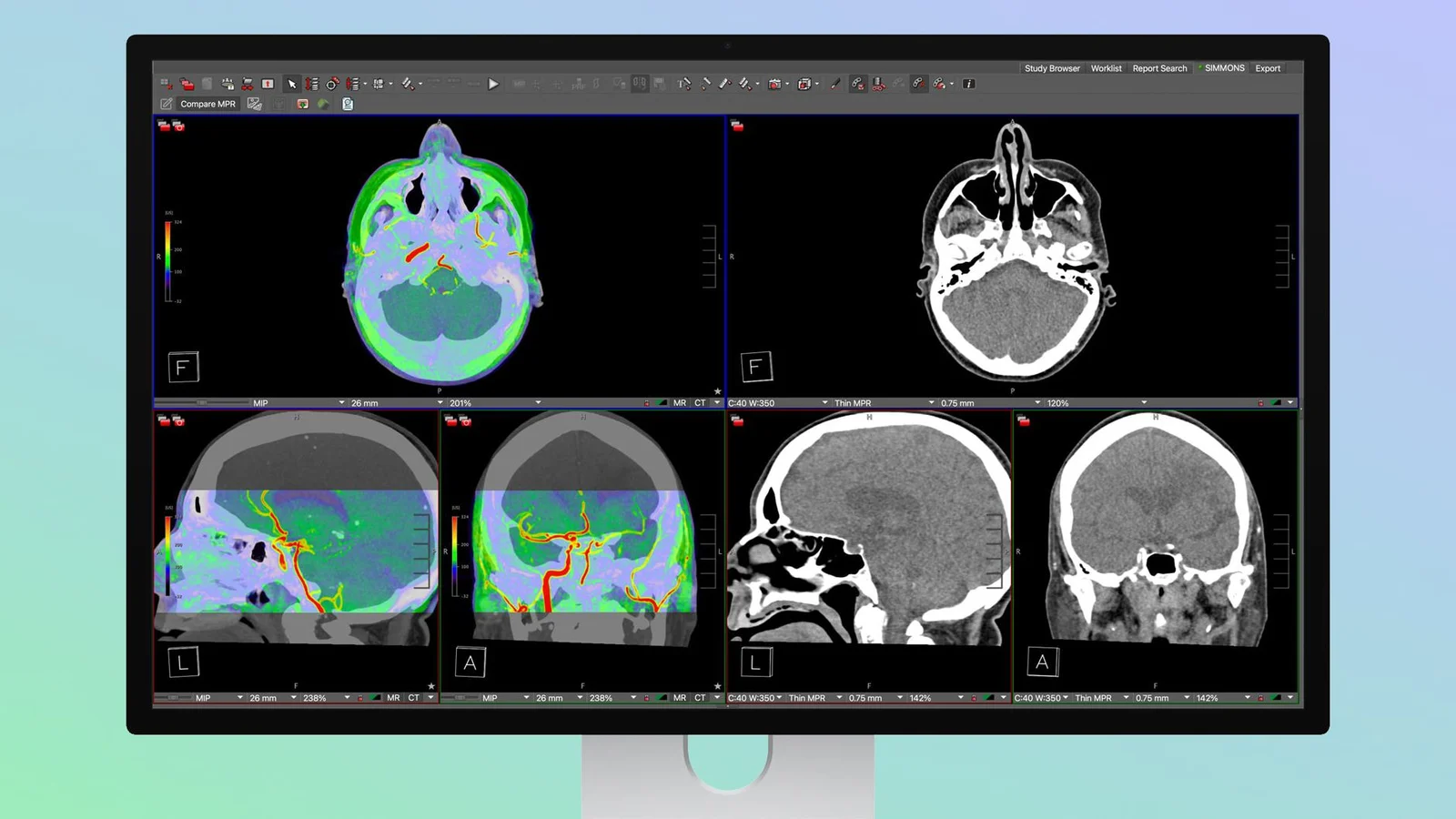
Apple Studio Display XDR Brings DICOM Imaging for Radiology
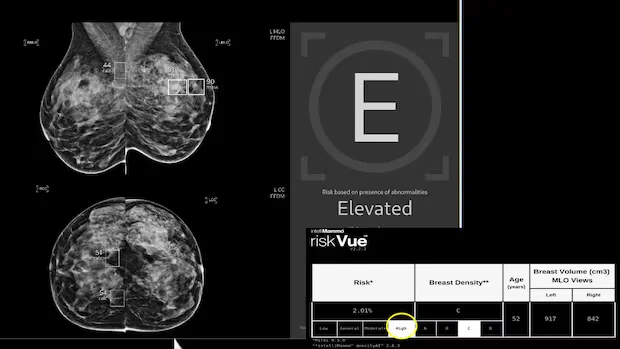
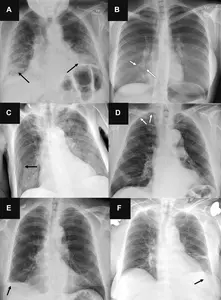
Apple's Studio Display XDR now supports DICOM medical imaging presets and a Medical Imaging Calibrator, enabling radiologists to view diagnostic radiology images on a high-end monitor; the calibrator is pending FDA clearance and should be available in the US soon. Pre-orders begin March 4 with a March 11 launch. The display features mini-LED backlighting, 2,304 local dimming zones, 2000 nits peak brightness, a 1,000,000:1 contrast ratio, and a 120Hz refresh rate, with a starting price of $3,299, offering a more affordable option than many dedicated medical imaging monitors.