Long COVID's Prevalence and Risks Highlighted by New Studies and AI Insights
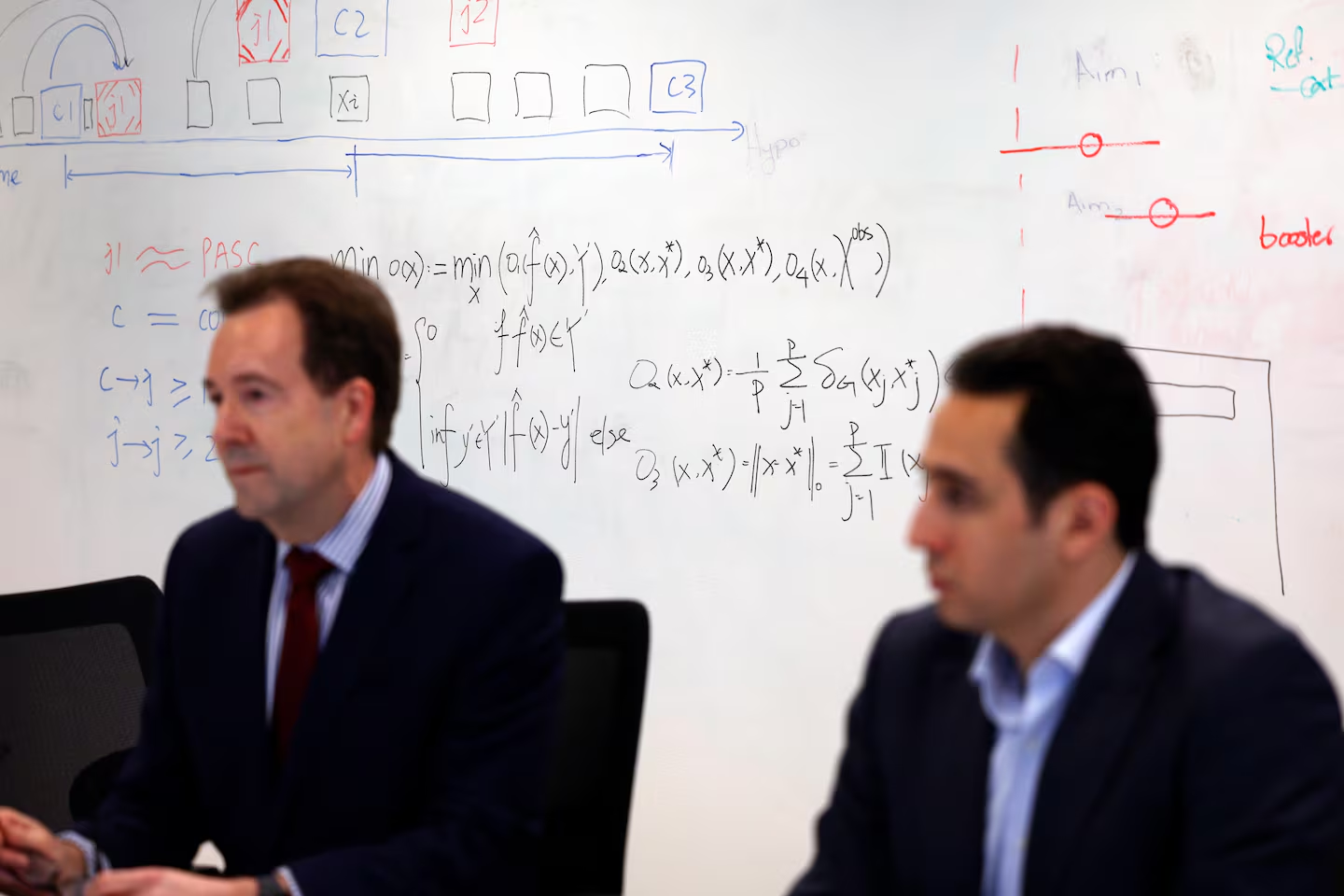
A new study suggests that long COVID may be more prevalent than previously thought, with an AI algorithm estimating that 22.8% of COVID-19 patients meet the criteria for long COVID, compared to the CDC's 6.9% estimate. The research, conducted by a team at Mass General Brigham, used AI to analyze electronic health records, but some experts question the findings due to the challenges in defining long COVID. The study highlights disparities in diagnosis and aims to refine treatment plans and further research on the condition.