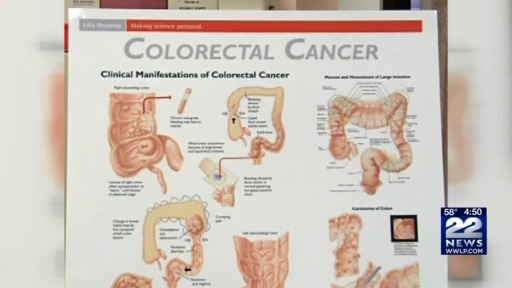
Colorectal cancer screening moves younger: why 45 is the new starting age and what to expect
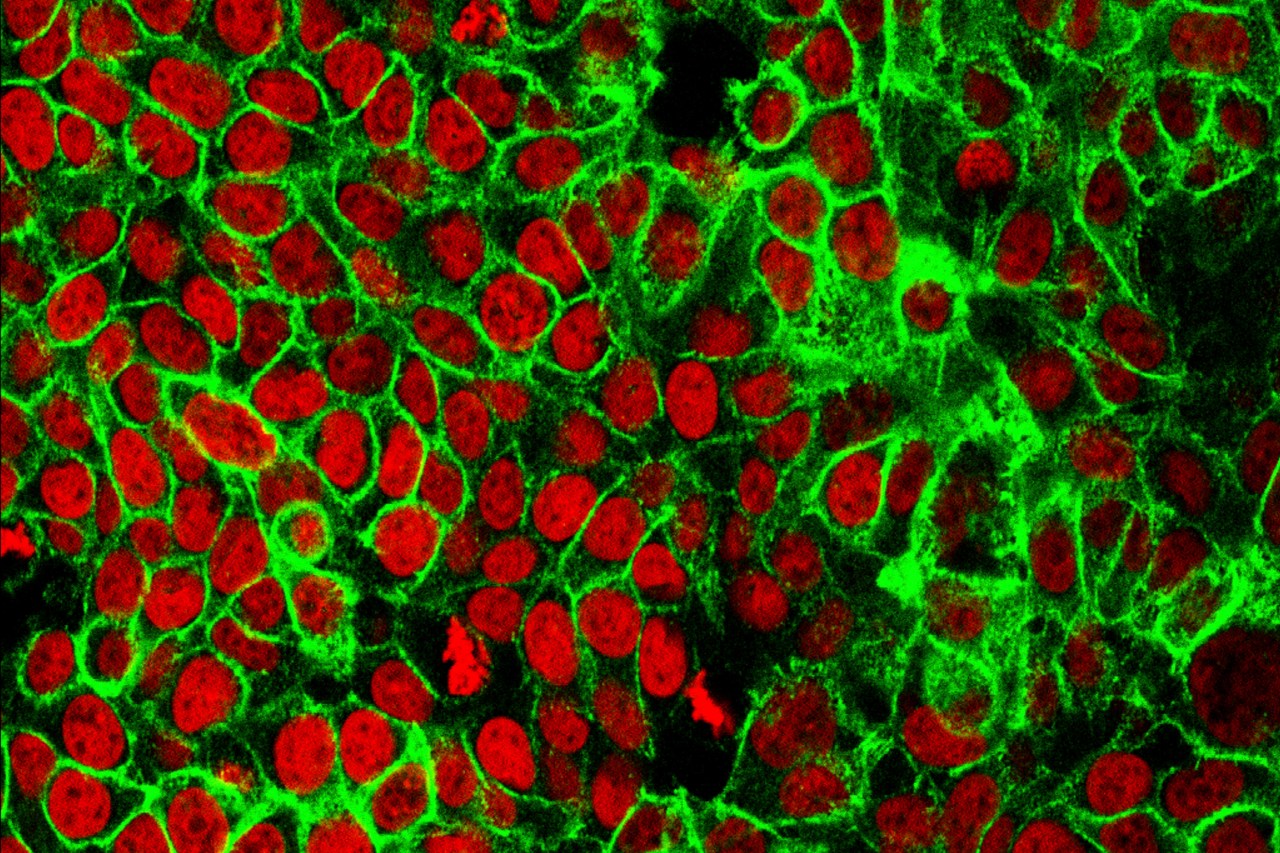
The piece explains that colorectal cancer is increasingly affecting younger people, leading to guidelines that now start average-risk screening at age 45 with a colonoscopy every 10 years (or stool tests as alternatives), notes that a family or personal history can trigger earlier testing, and discusses symptoms, costs, and the role of noninvasive tests like Cologuard and FIT. It also highlights that lifestyle factors and access to care influence risk and screening uptake.