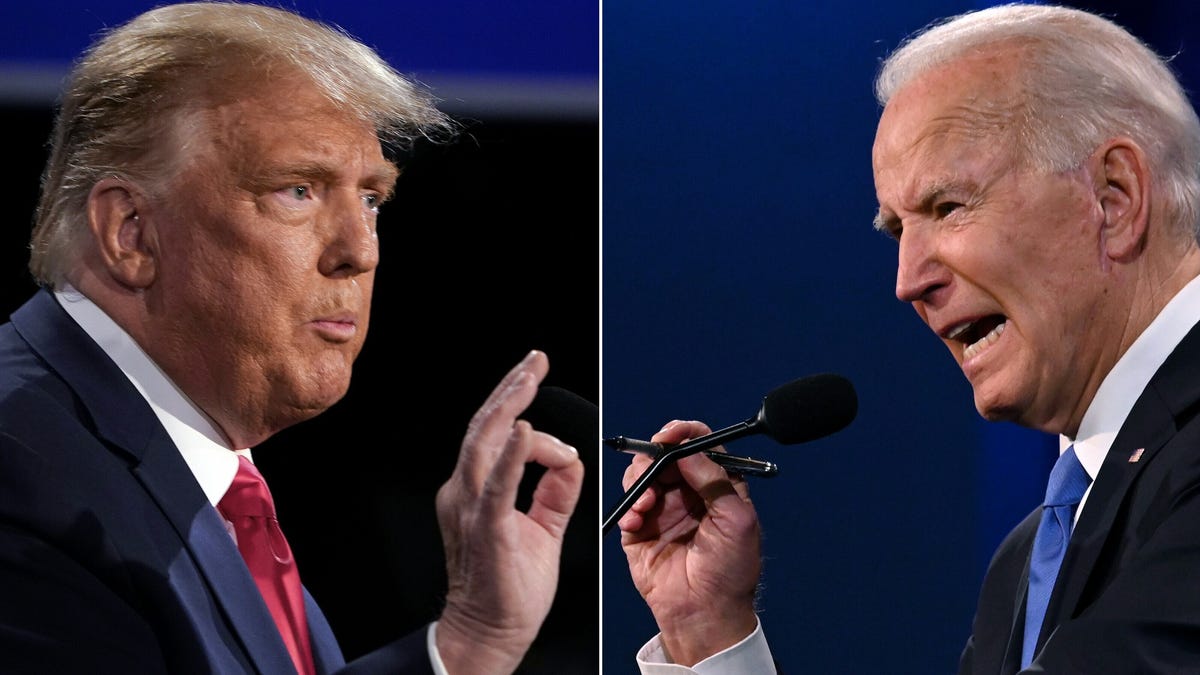
Biden Pushes for Medicare and Medicaid to Cover Weight-Loss Drugs
The Biden-Harris Administration has proposed a new rule to expand Medicare and Medicaid coverage for anti-obesity medications, aiming to make these treatments more affordable for millions of Americans. This initiative is part of a broader effort to lower prescription drug costs and improve health outcomes, building on previous legislation like the Inflation Reduction Act. The proposal could significantly reduce out-of-pocket expenses for these medications, which are crucial for managing obesity-related health risks.