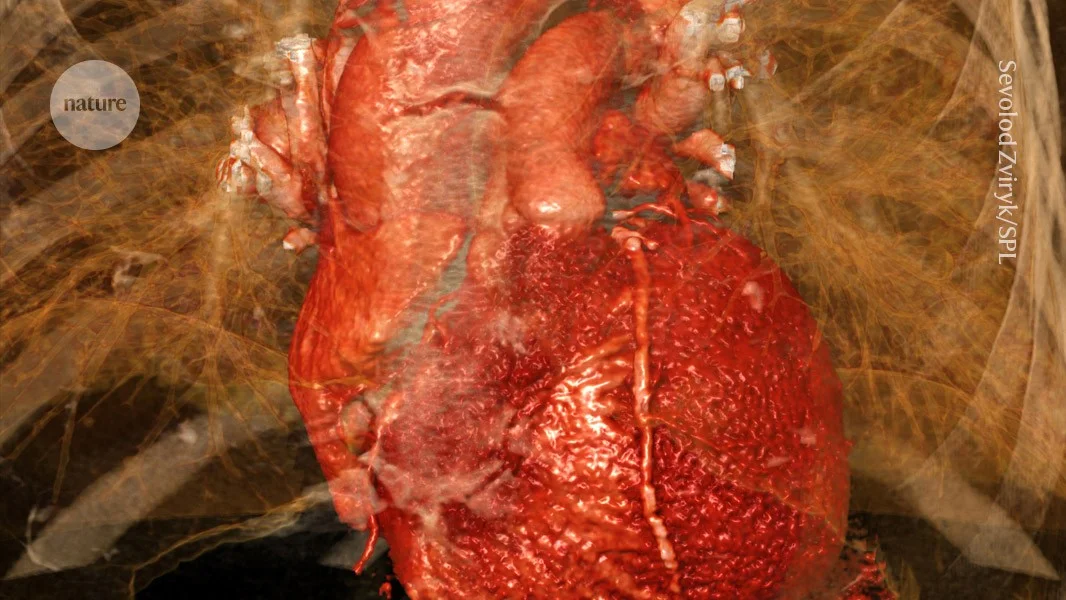
Brain–heart–immune axis drives heart damage after a heart attack, mouse study finds
A mouse study published in Cell shows that signals from the heart to the brain activate a vagus-mediated brain–immune circuit that worsens tissue damage after a heart attack; inhibiting this pathway reduced injury and improved heart function, suggesting new therapeutic targets.









