Patch Shortage Tests Access to Menopause Hormone Therapy
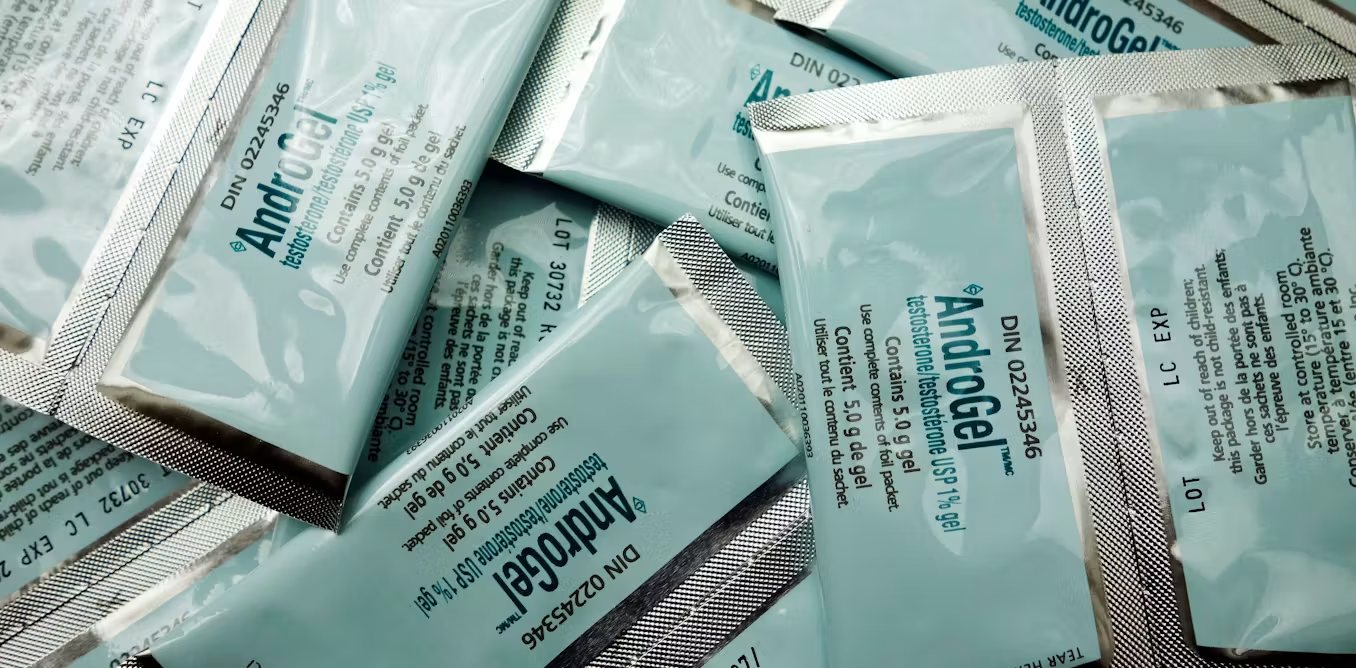
Rising demand for menopause hormone therapy—accelerated by FDA label changes and greater public awareness—is outpacing the supply of estrogen transdermal patches, leading to intermittent stockouts, patient brand-switching, and higher costs. Doctors are advising alternatives (other patches, gels, pills) and working with manufacturers to increase capacity as supply catches up.