Measles resurges as vaccination gaps threaten child health
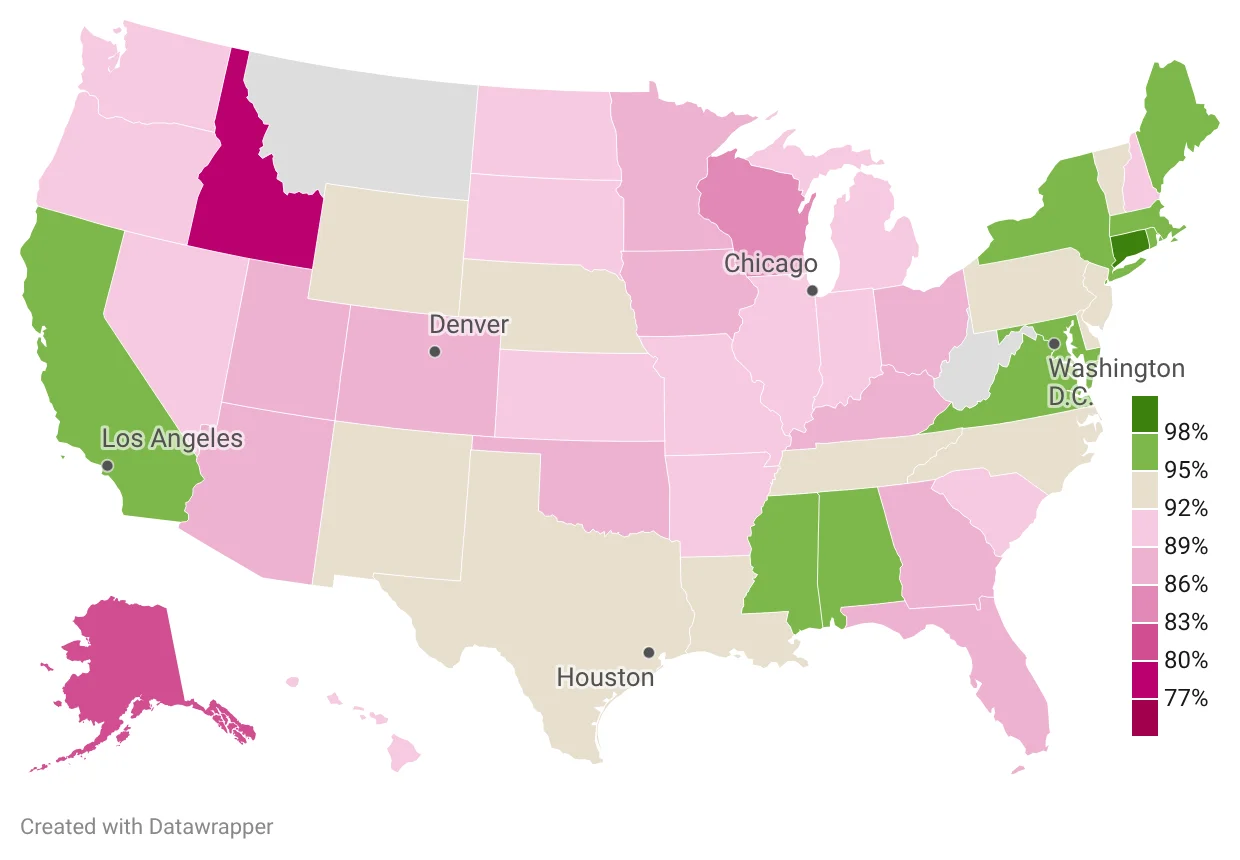
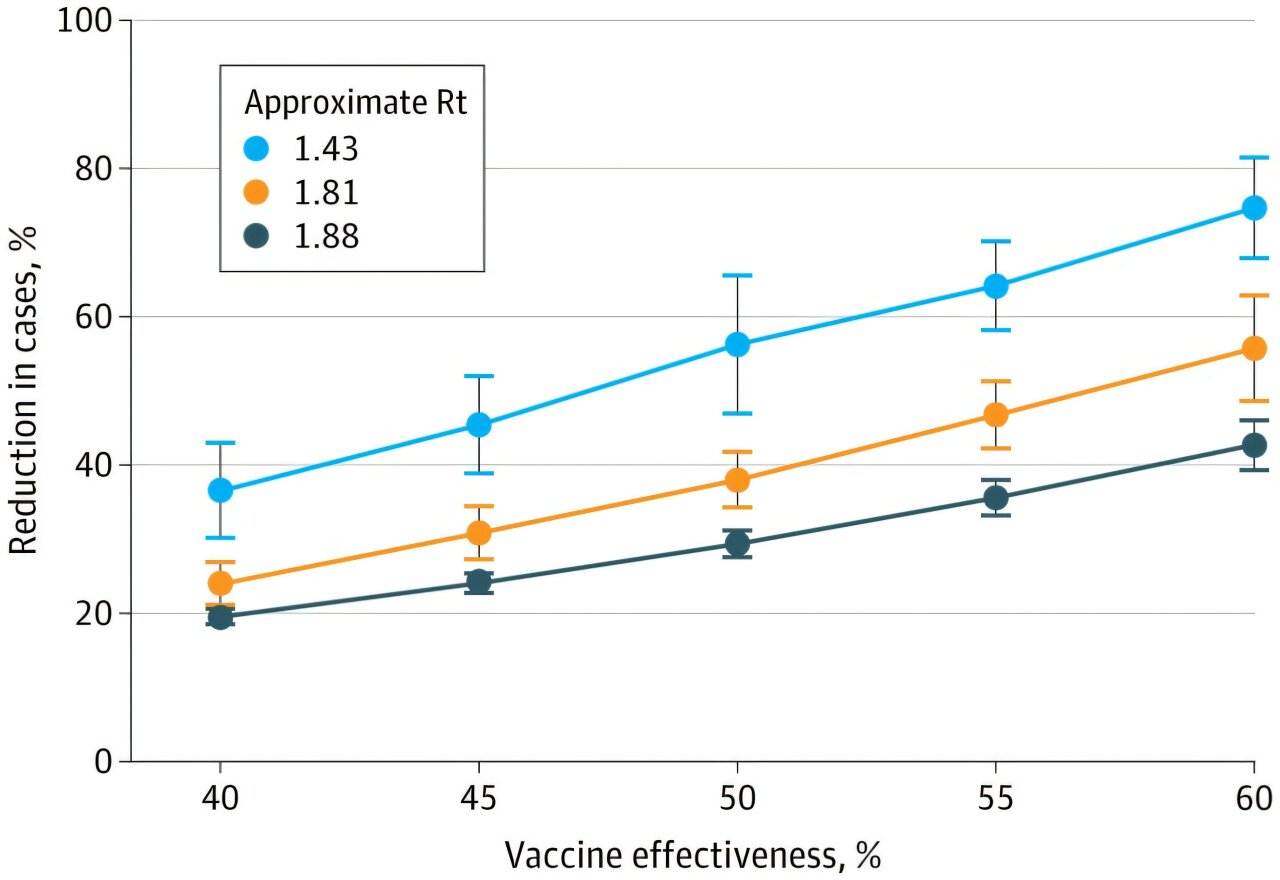
London is grappling with a measles outbreak affecting unvaccinated children under 10, reflecting a global rise after six countries lost their measles-free status. Measles is highly contagious and spreads through coughs and sneezes, with no specific treatment; vaccination is the key defense. The WHO notes a 95% herd-immunity threshold, but UK two-dose coverage stood around 84% in 2024 (with 2,911 confirmed England cases that year). Vaccines (MMR/MMRV) provide strong protection, and public health guidance emphasizes ventilation, hygiene, and avoiding shared items to curb transmission. High-risk groups include babies and the immunocompromised, and complications can include pneumonia, brain inflammation, or, in pregnancy, miscarriage/stillbirth.