Long COVID Brain Fog Tied to Lung Function and Cognitive Decline
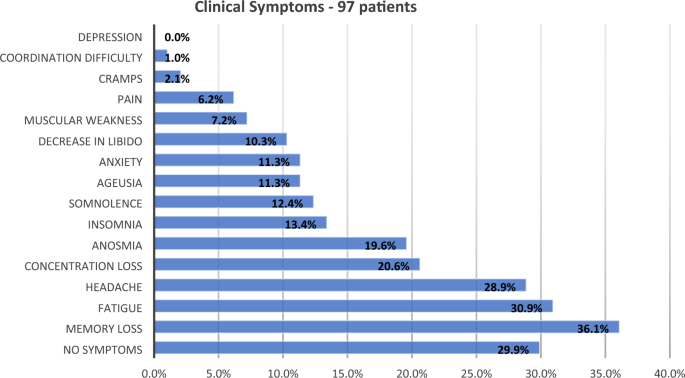
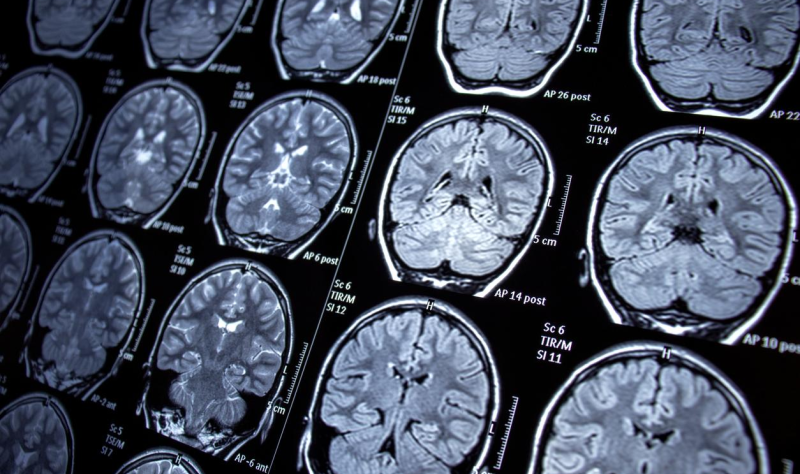
A study by University of Iowa researchers suggests that sluggish gas exchange in the lungs may contribute to brain fog in long COVID patients. Using MRI to assess lung and brain function, the study found a potential link between impaired pulmonary gas exchange and cognitive dysfunction, as well as reduced brain gray- and white-matter volumes. The findings indicate that improving gas exchange could be a potential treatment strategy for cognitive issues in long COVID.