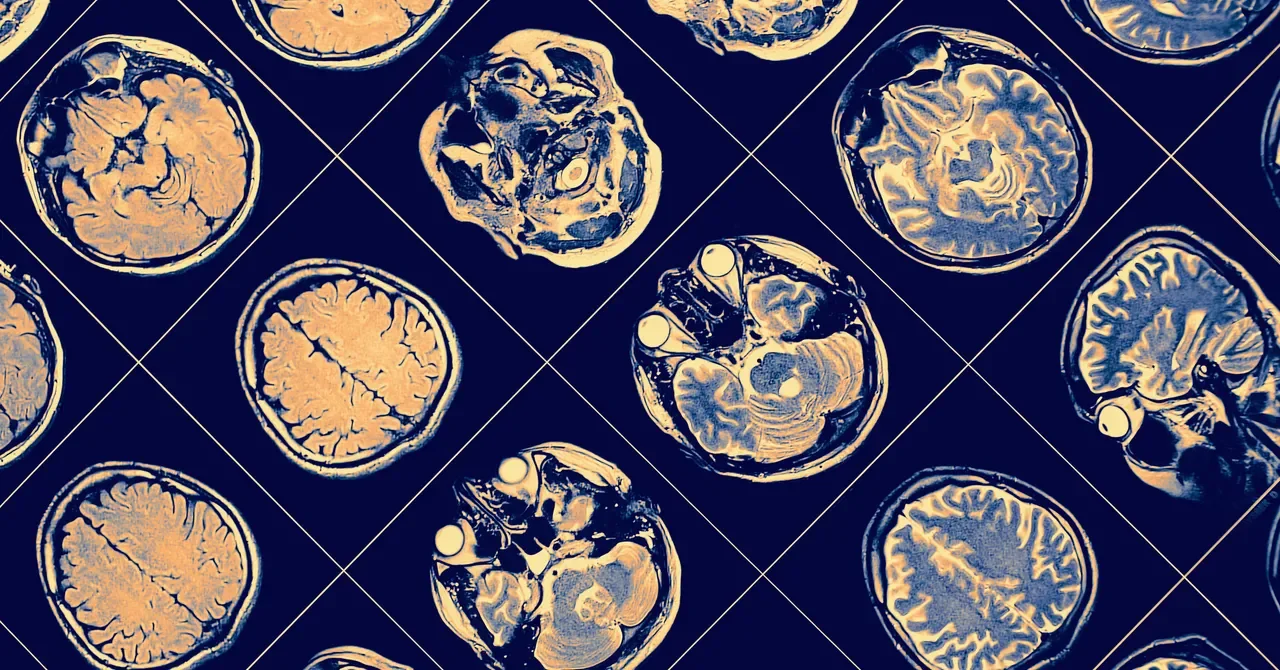
Dementia Patients Still Prescribed Risky Brain-Active Drugs, Study Finds
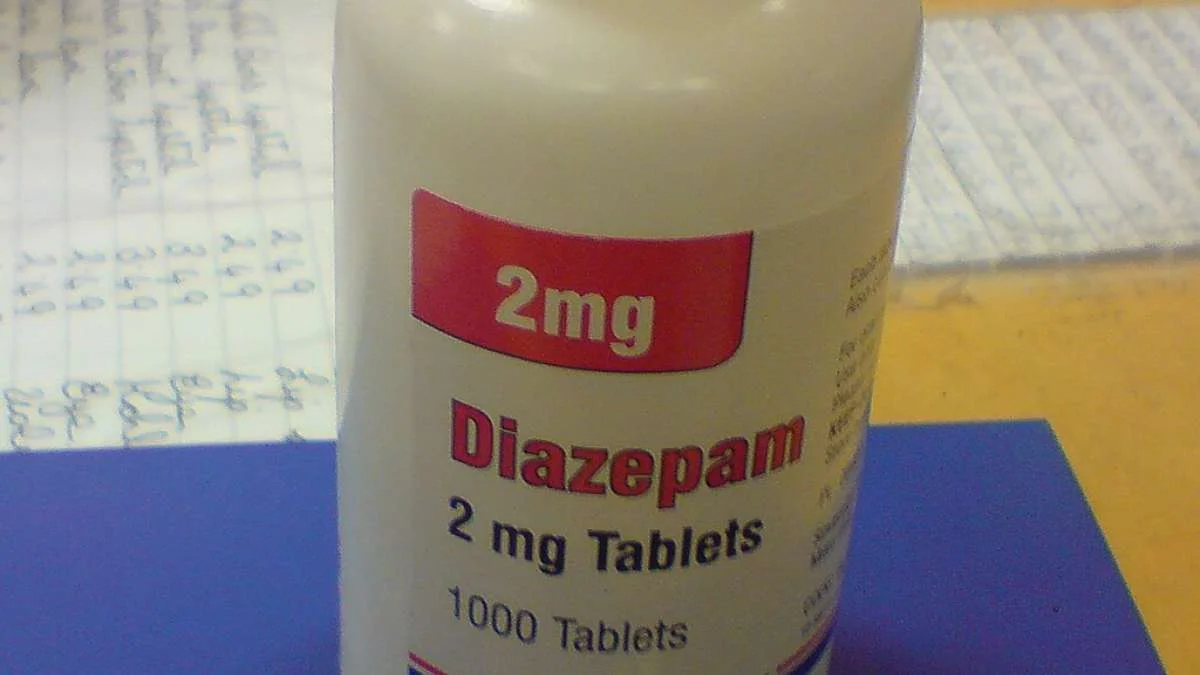
A UCLA-led analysis of Health and Retirement Study linked to Medicare claims finds that about 25% of older adults with dementia receive brain-altering CNS medications, with two-thirds lacking a documented clinical indication in 2021; while overall inappropriate CNS prescribing fell from 15.7% to 11.4% and benzodiazepine and sleep-drug use declined, antipsychotic prescriptions rose from 2.6% to 3.6%, underscoring persistent safety risks for vulnerable seniors and the need to taper or stop these medications when not clearly indicated.