Could autism be preventable in some cases through early-life exposures?
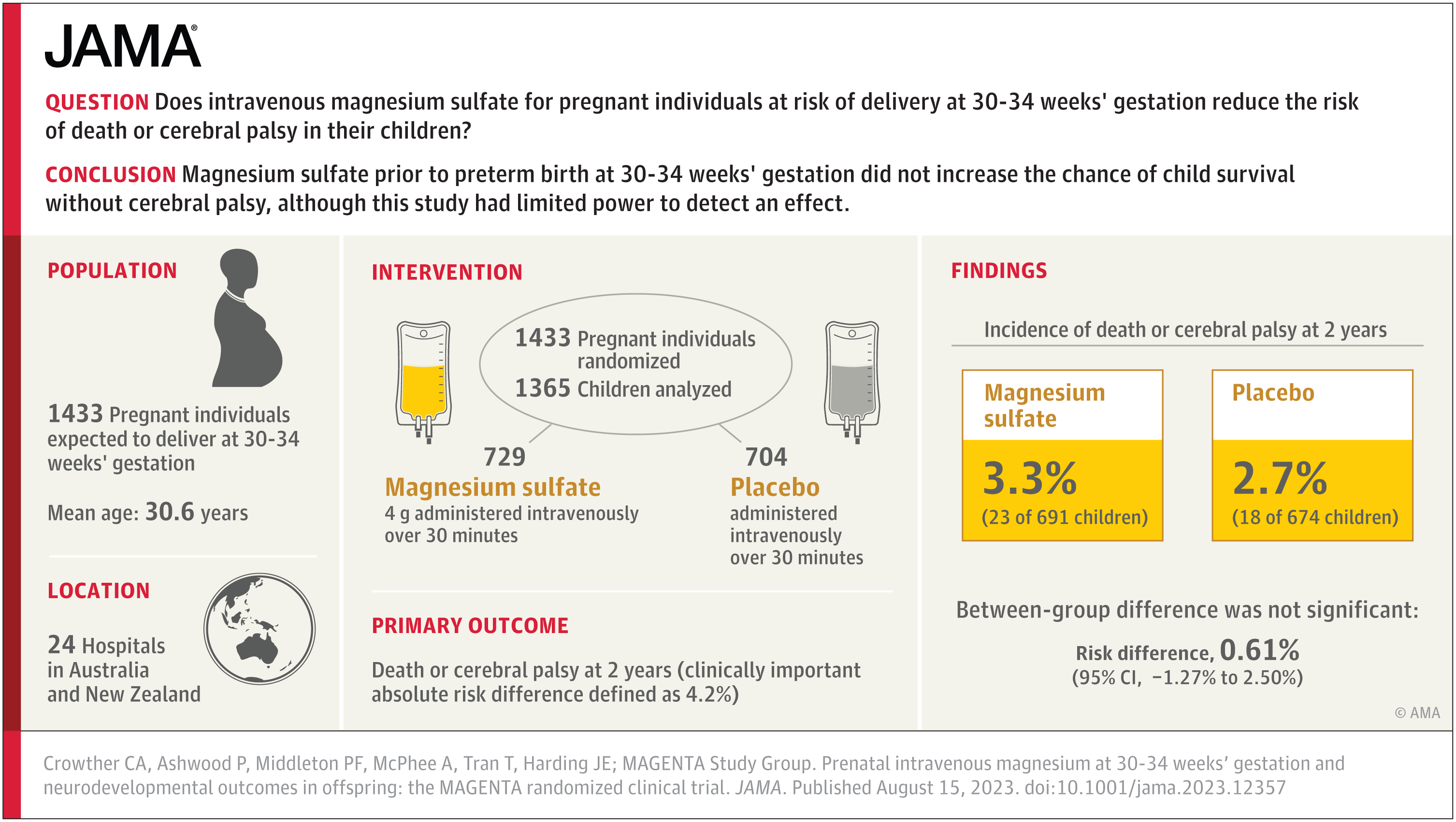
Some scientists are exploring whether avoiding environmental exposures before conception and in early life—the so‑called 'trimester zero' window—could lower autism risk in some children. While still in early stages, obstetricians like Jeanne Conry point to a 1,300‑day window (from preconception through a child’s second birthday) during which nutrition and lifestyle may influence autism risk, suggesting potential, non-guaranteed prevention rather than definitive outcomes.