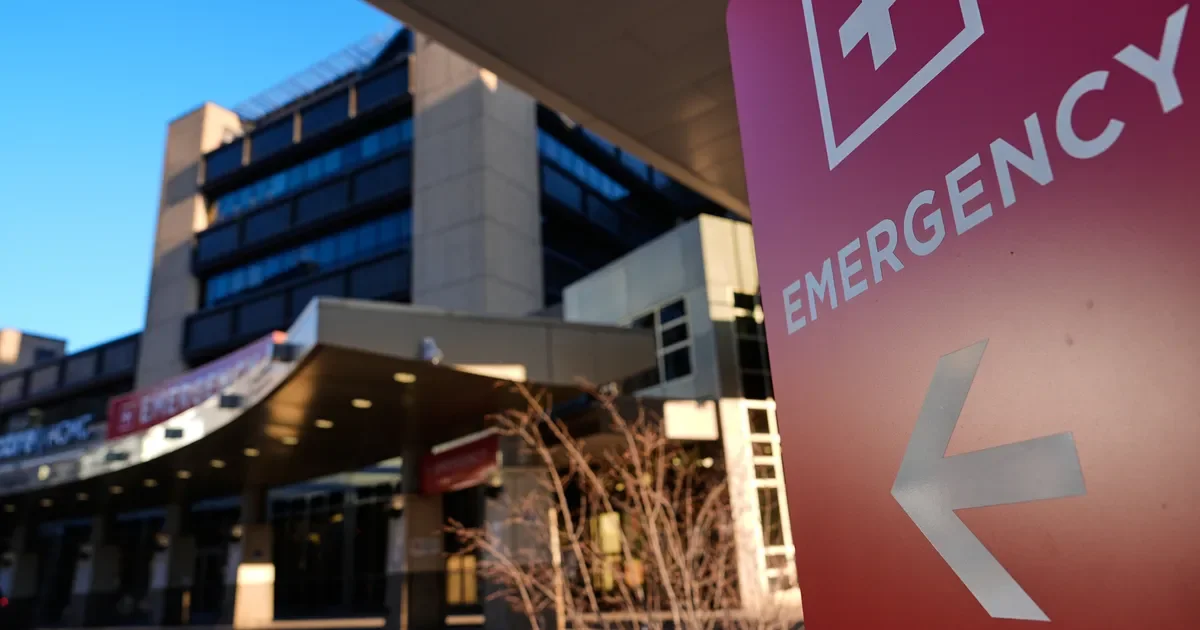
Nurses challenge ICE’s injury claim as detainee’s skull fractures spark hospital tensions in Minneapolis
Nurses at Hennepin County Medical Center say ICE’s claim that a Mexican detainee fractured his skull by running headfirst into a wall while handcuffed is implausible, noting injuries that don’t fit a fall or wall impact. The dispute highlights friction between federal agents and hospital staff, with ICE remaining at the bedside and hospital protocols evolving to limit interactions. The detainee was treated, later discharged with memory loss and long recovery ahead, and a court ordered his release from ICE custody.