Two Everyday Habits Drive Most Preventable Cancers, Study Finds
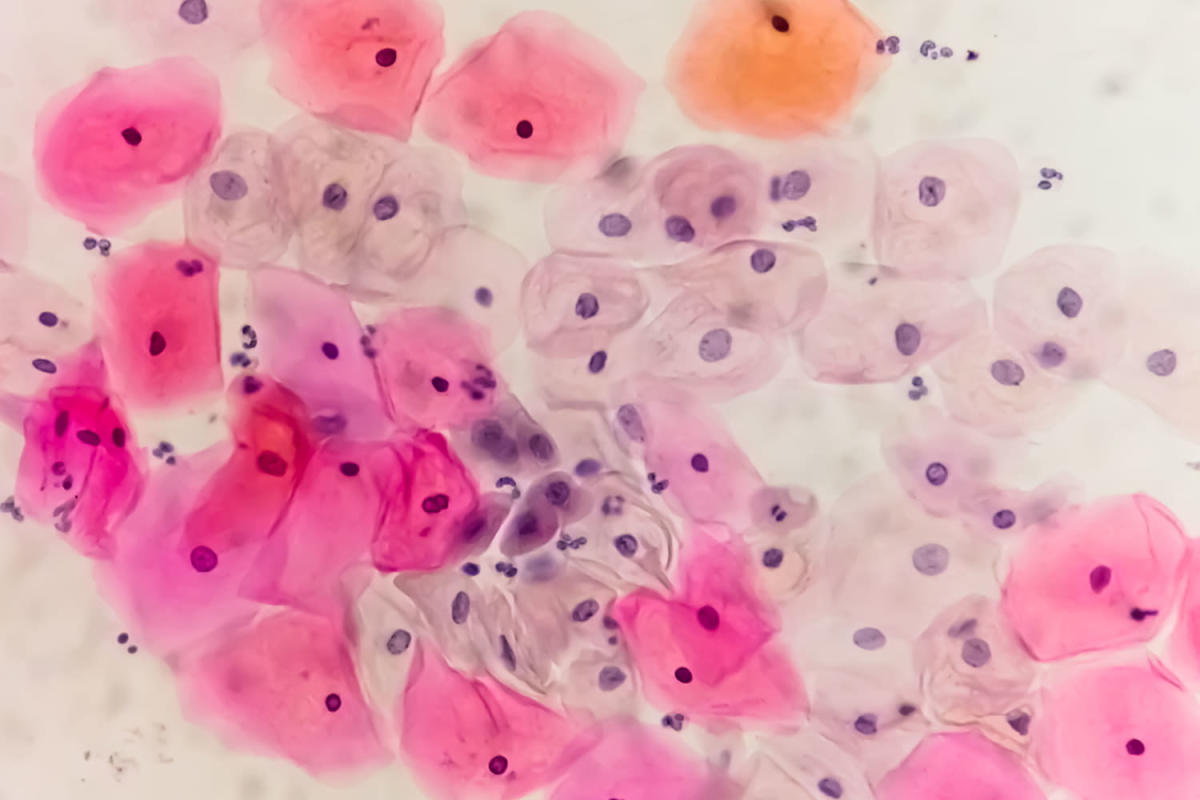
A Nature Medicine study links the majority of preventable cancers to two everyday habits—smoking and alcohol—while also noting roles for obesity, physical inactivity, air pollution, and HPV infection; the findings emphasize actions like quitting smoking, reducing alcohol, maintaining a healthy weight and activity, and HPV vaccination to lower cancer risk globally.