Could ibuprofen lower some cancer risks? Early findings with caveats
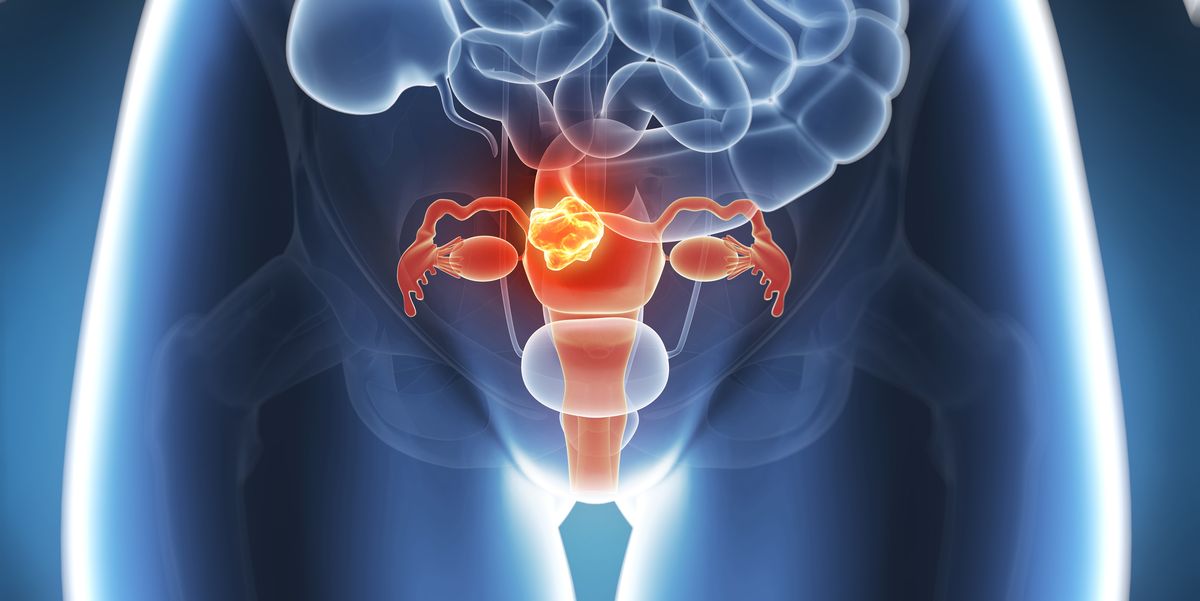
Emerging studies link regular ibuprofen use with lower risks of endometrial and bowel (colorectal) cancers, possibly by dampening inflammation and affecting cancer-related genes, though evidence is not conclusive and high-dose or long-term NSAID use can cause serious side effects. Experts caution against self-prescribing ibuprofen for cancer prevention and emphasize proven prevention strategies like a healthy weight, exercise, and a balanced diet.