Scientists Warn of Growing Drug Resistance in Common Infections
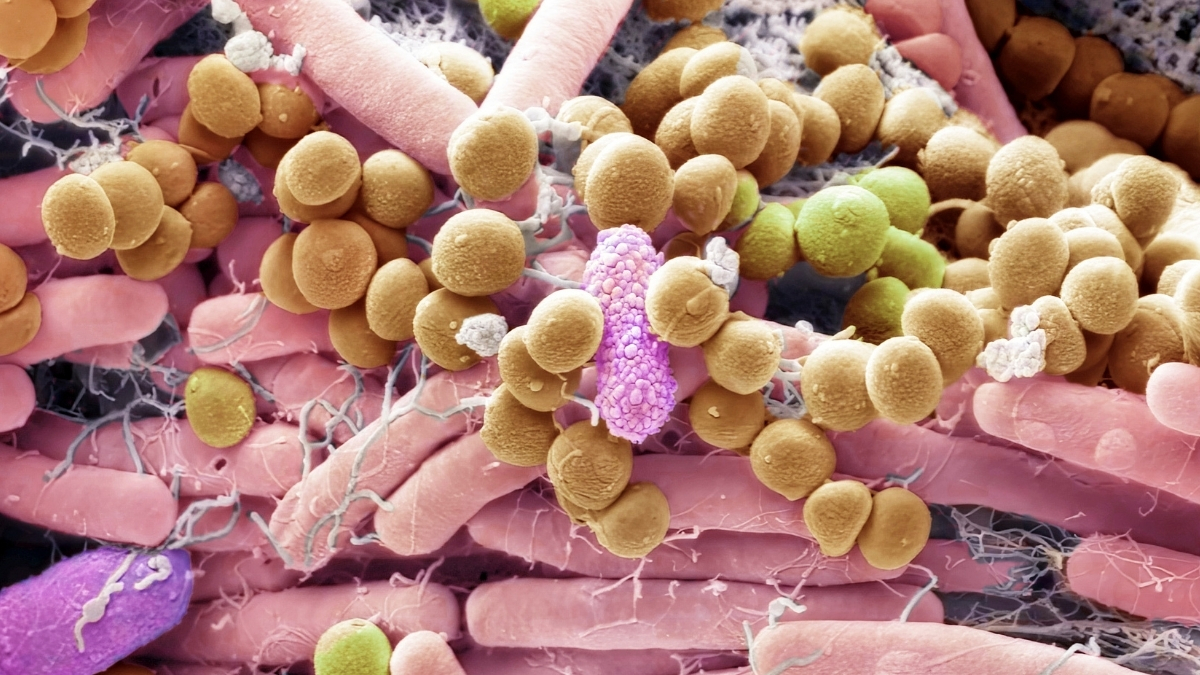
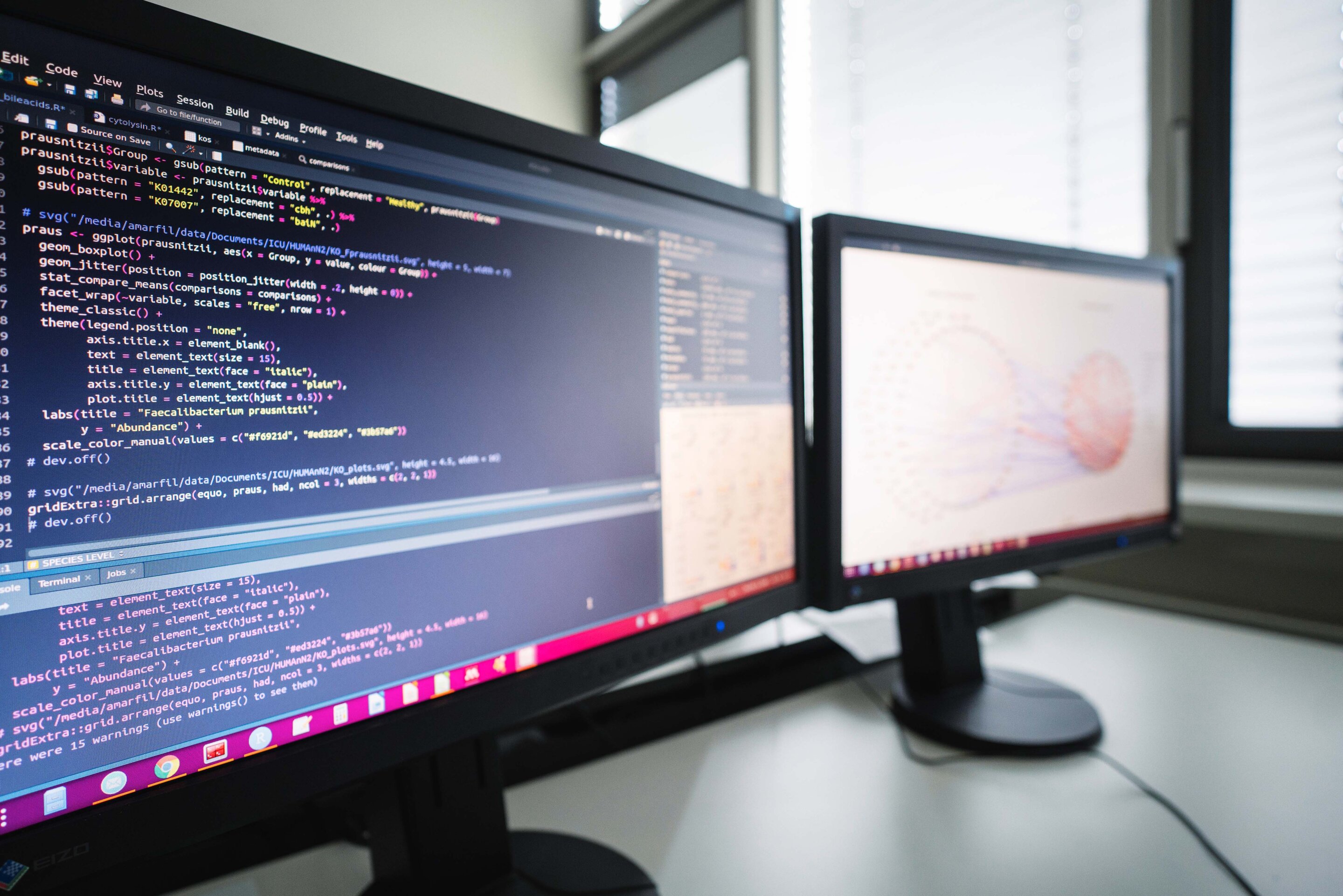
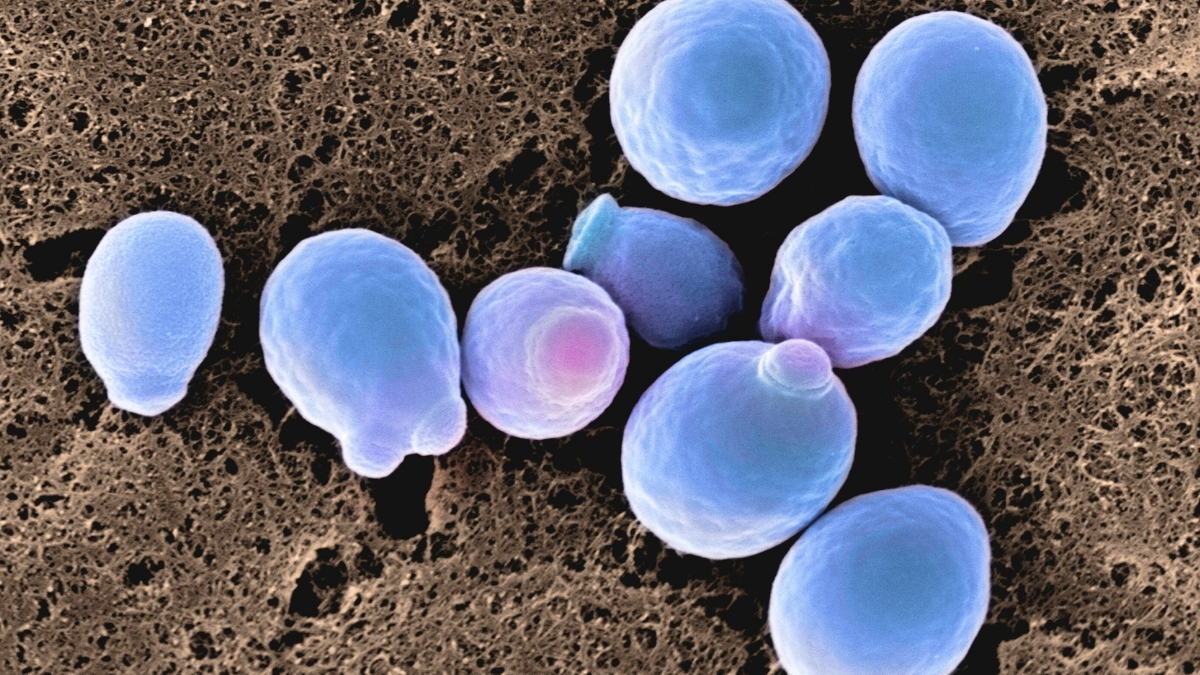
The article warns that common fungal infections like thrush are increasingly resistant to antifungal drugs due to factors like misuse, environmental changes, and Candida's adaptability, making treatment more challenging and highlighting the importance of good hygiene and microbiome health to prevent resistant strains.