"U.S. Measles Cases Surge, Urgent Call for Vaccination"
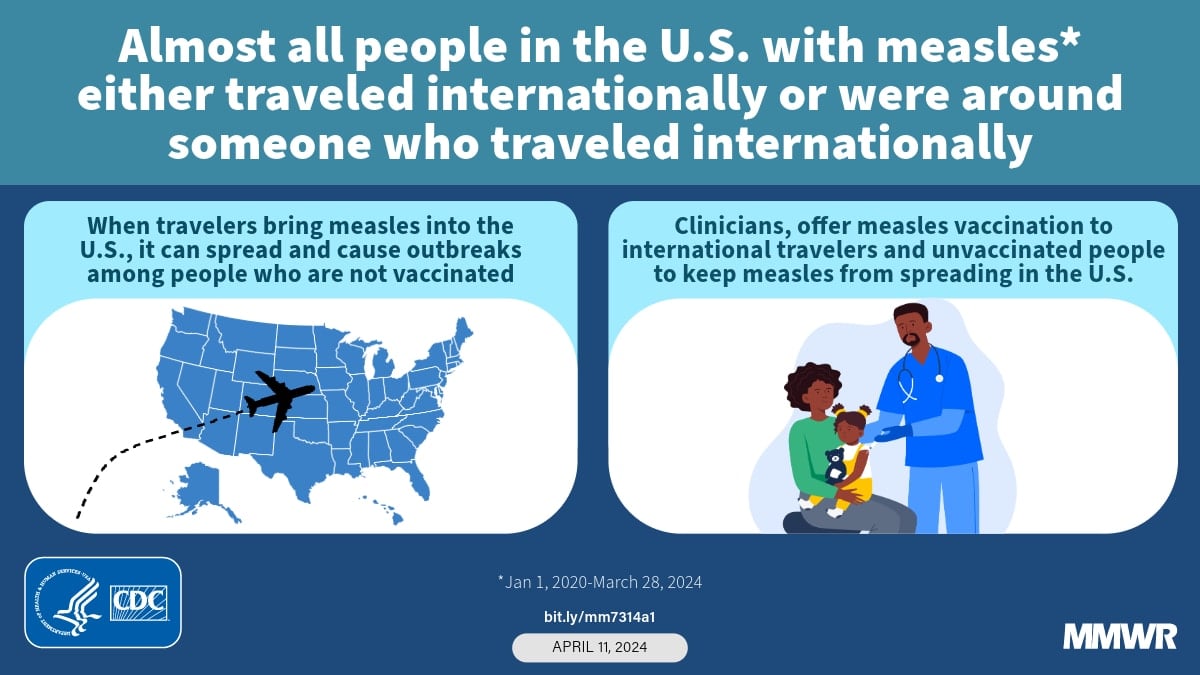
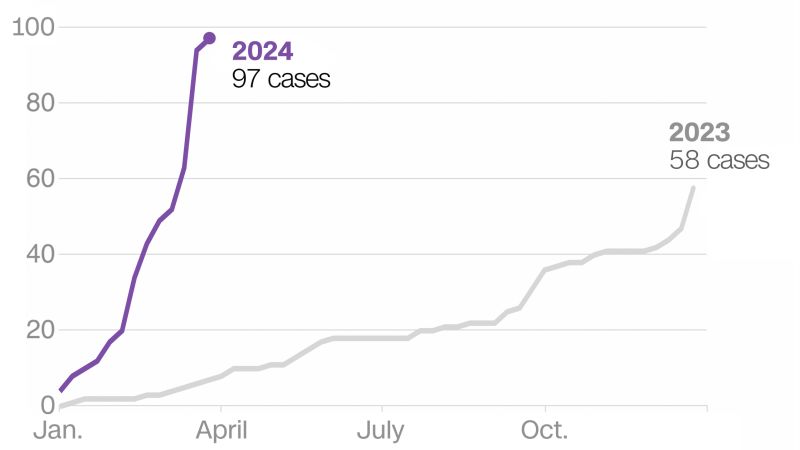
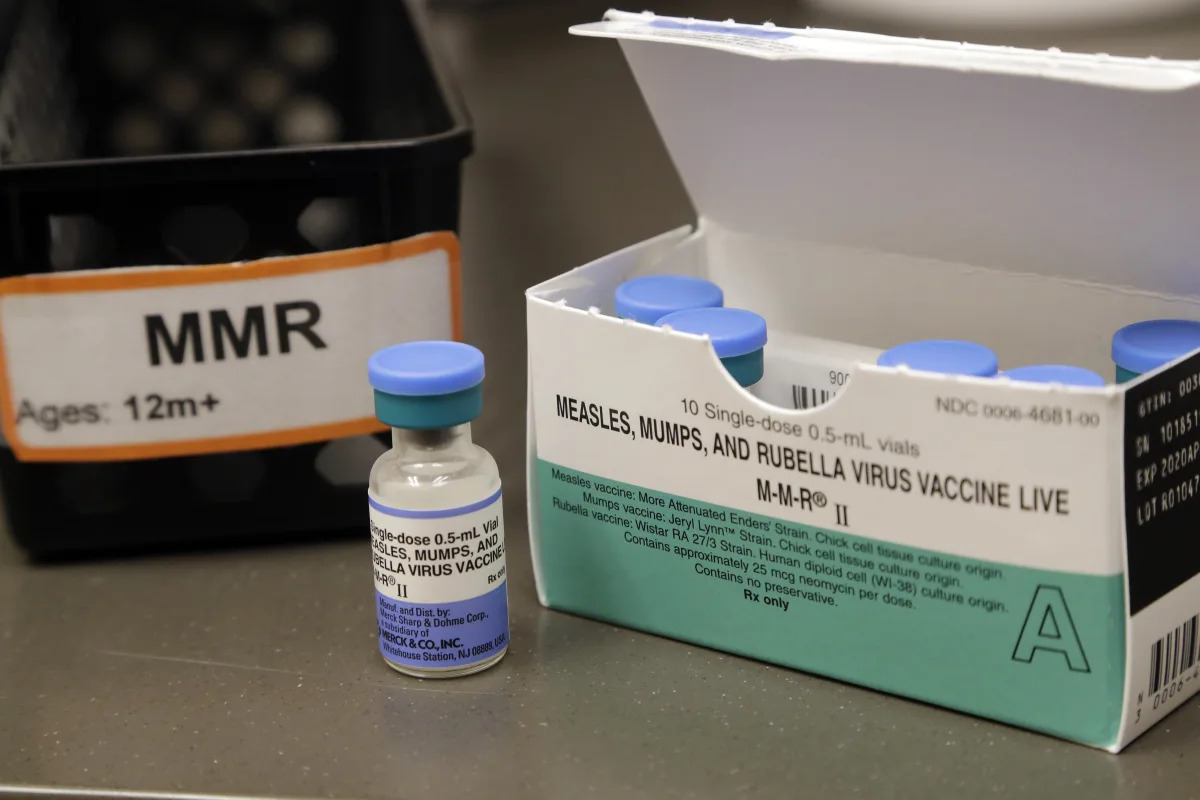
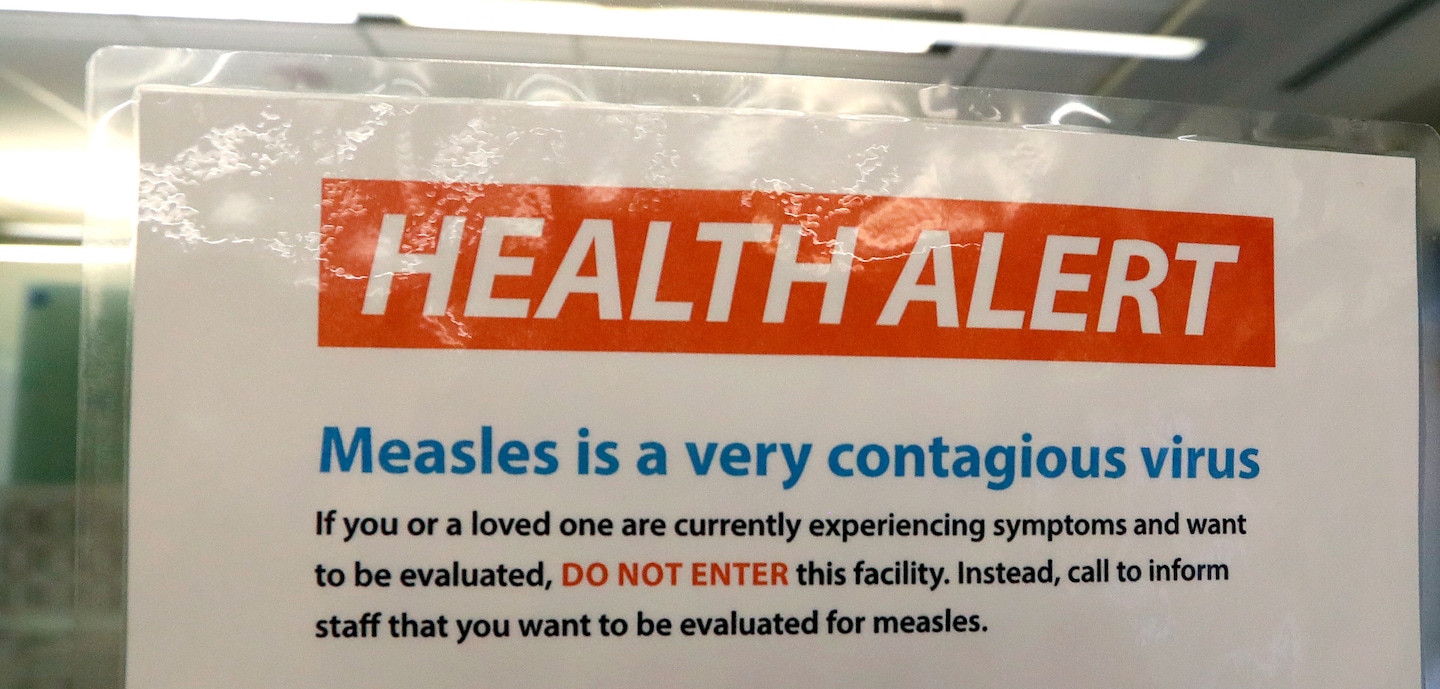
Measles cases in the United States are on track to be the worst since 2019, with anti-vaccine activists contributing to vaccine hesitancy. Measles is highly contagious and can cause serious complications, but can be prevented with the measles, mumps, and rubella vaccine. Vaccination rates are falling globally, leading to outbreaks in multiple countries, including the United States. Vaccine hesitancy is being fueled by activists and social media, despite the proven effectiveness of vaccines in preventing measles. The battle against measles requires a concerted effort to boost vaccination rates and combat misinformation.