New Blood Thinner May Replace Aspirin for Heart Attack Prevention
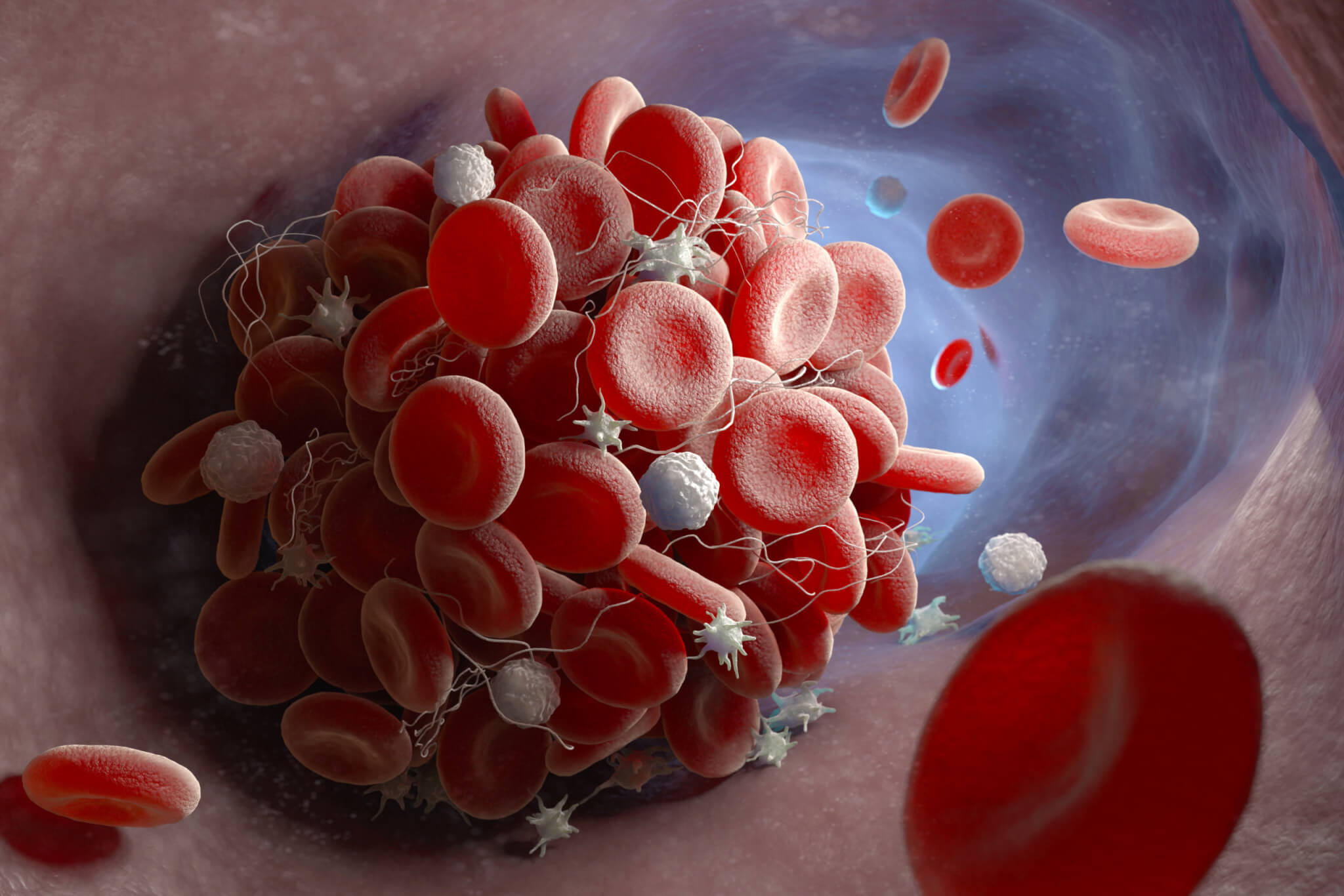
A review suggests that switching from aspirin to the blood thinner clopidogrel can reduce the risk of heart attack, stroke, or death by 14% in patients with coronary heart disease, with similar safety profiles and potential cost benefits, prompting calls for updated treatment recommendations.