"Uncovering Hidden Fees: How Insurance Companies Profit at Patients' Expense"
TL;DR Summary
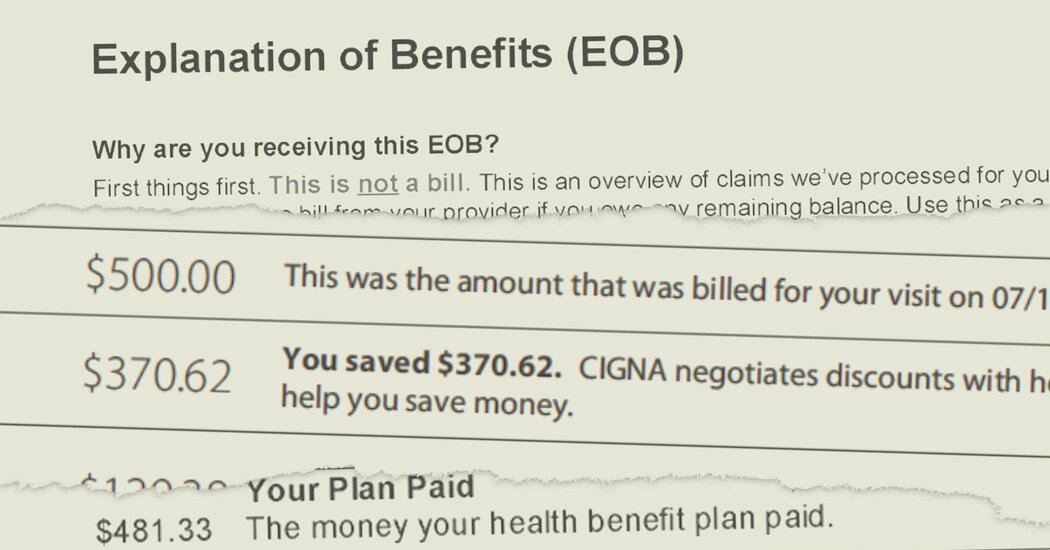
A little-known data firm called MultiPlan helps health insurers maximize profits by negotiating lower payments for out-of-network claims, leaving patients responsible for the remaining balance. This practice has resulted in patients receiving unexpected bills amounting to tens of thousands of dollars, despite having insurance coverage. MultiPlan and insurers typically receive a percentage of the "savings" on each claim, creating a financial incentive to recommend lower payments. Confidential pricing and fee data, as well as insurance statements, have shed light on the extent of these hidden fees and the impact on patients.
Insurance Companies Reap Hidden Fees as Patients Get Unexpected Bills The New York Times
Reading Insights
Total Reads
0
Unique Readers
10
Time Saved
2 min
vs 3 min read
Condensed
81%
491 → 91 words
Want the full story? Read the original article
Read on The New York Times