Houston Doctor Indicted for Falsifying Records to Deny Liver Transplants
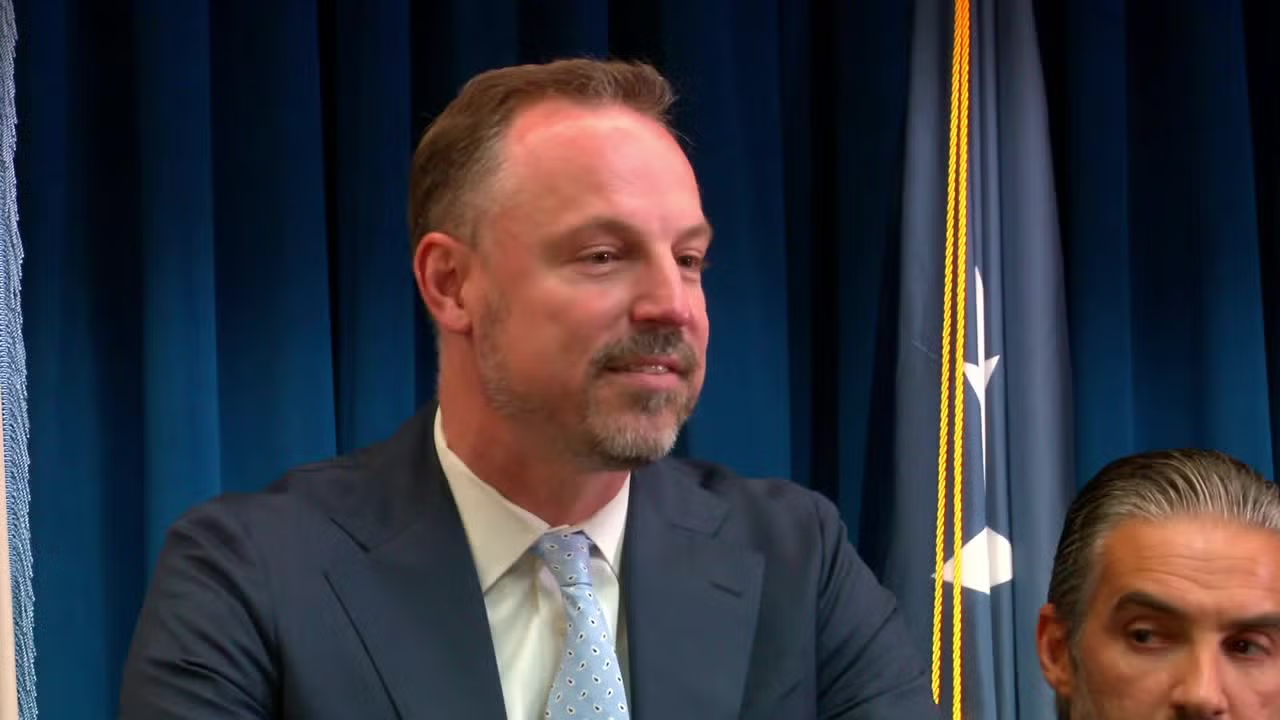
A Houston surgeon, Dr. John Stevenson Bynon Jr., was indicted on five counts of false statements in health care matters for allegedly falsifying medical records to render five patients ineligible for liver transplants; among them, three died and two later received livers at other hospitals. The case prompted Memorial Hermann to temporarily shut down its transplant program, which later reactivated; if convicted, he faces up to five years and a $250,000 fine per count.