Insurers, including Arkansas Blue Cross and Blue Shield, refuse coverage for groundbreaking Alzheimer's drug
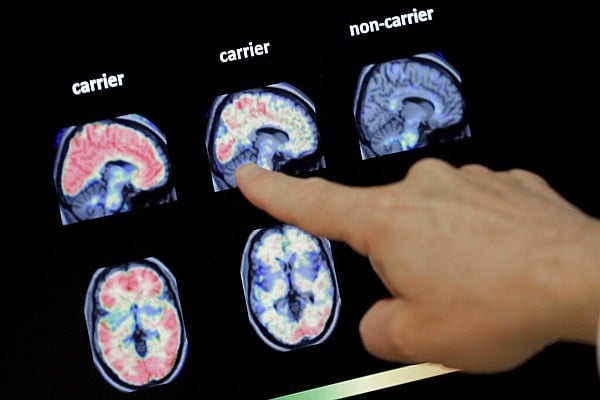
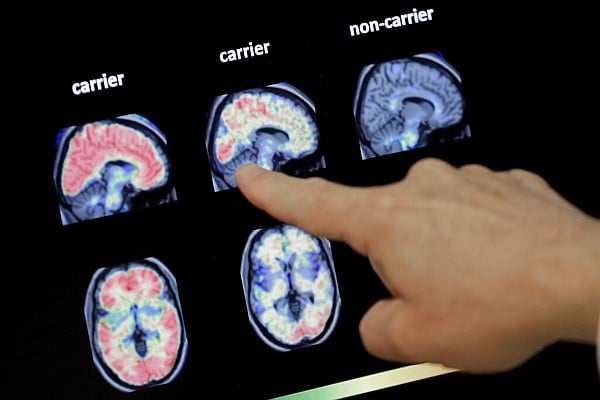
Arkansas Blue Cross and Blue Shield, the largest health insurance company in Arkansas, has decided not to cover the Alzheimer's drug Leqembi, citing insufficient evidence of its effectiveness and concerns about its risks. The decision also applies to the health plans covering state and public school employees. The drug, which costs $26,500 a year plus additional clinic administration fees, became the first to win full approval from the FDA for slowing the progression of Alzheimer's. Medicare, the U.S. Veterans Health Administration, Arkansas' Medicaid program, and United Healthcare's standard commercial plans have opted to cover the drug. Advocates are urging insurers to reconsider their coverage decisions.